"Coronary Heart Disease Uncovered: How It Starts, How to Stop It, and How to Protect Your Heart for Life"
BlogThis in-depth, evidence-based article explores coronary heart disease (CHD) from its earliest stages to advanced prevention strategies. Written in a clear, accessible style by a medical expert, it explains how CHD develops, the role of risk factors like high cholesterol, hypertension, diabetes, and smoking, and the underlying biological mechanisms that damage the arteries. It also examines cutting-edge research, lifestyle changes, and medical treatments that can prevent or slow the disease’s progression. Backed by reputable scientific sources, this comprehensive guide empowers readers with practical knowledge to protect their heart health and reduce their risk of cardiovascular complications for life.
DISEASES
8/13/202530 min read
1 – Introduction: Understanding Coronary Heart Disease (CHD)
Coronary Heart Disease (CHD) — also known as coronary artery disease (CAD) or ischemic heart disease (IHD) — is the most common form of heart disease and the single leading cause of death worldwide. According to the World Health Organization (WHO), more people die from CHD each year than from any other condition — over 17.9 million deaths annually are linked to cardiovascular diseases, and CHD alone is responsible for nearly half of these.
What Exactly Is CHD?
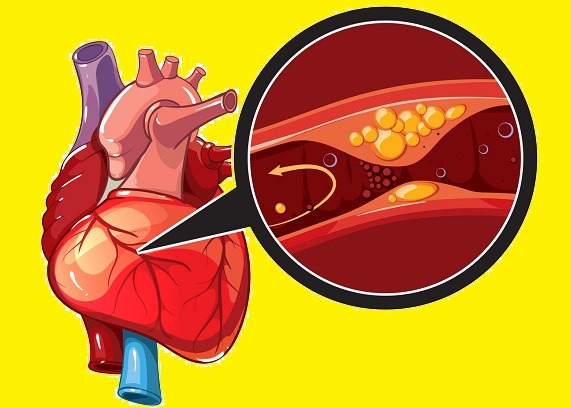
To understand CHD, imagine the heart as a house that needs constant electricity to function. The “wires” carrying this electricity are your coronary arteries — blood vessels that supply oxygen and nutrients to every cell of the heart muscle. If these arteries become narrowed or blocked, the heart’s power supply is interrupted. Without enough oxygen-rich blood, parts of the heart muscle cannot function properly, leading to symptoms such as chest pain (angina) or, in severe cases, heart attacks (myocardial infarctions) that can be fatal.
How Does CHD Develop?
The most common cause of CHD is atherosclerosis — a slow, progressive process where fatty deposits called plaques build up inside the artery walls. Over time:
Plaques can harden and narrow the arteries, restricting blood flow.
If a plaque ruptures, the body tries to “repair” it by forming a blood clot.
This clot can block the artery entirely, cutting off blood flow to part of the heart.
This process doesn’t happen overnight. It often begins in childhood or teenage years, silently progressing for decades before symptoms appear.
Why Is CHD So Important?
CHD is not just a disease for the elderly. In fact, studies show that early artery changes can start in the teenage years, especially in people who smoke, eat poorly, or are overweight.
Economic impact: In the U.S., CHD costs over $200 billion annually in healthcare expenses, lost productivity, and medications (CDC, 2024).
Quality of life impact: CHD can limit a person’s ability to work, exercise, and enjoy daily activities.
Emotional impact: Living with CHD often brings stress, anxiety, and depression, both for patients and their families.
A Global Pattern
In high-income countries, deaths from CHD have declined in recent decades thanks to better prevention (less smoking, improved diet) and advanced treatments (angioplasty, bypass surgery, statins).
In low- and middle-income countries, CHD rates are rising rapidly because of urbanization, fast-food diets, reduced physical activity, and limited healthcare access.
The Preventable Nature of CHD
Here’s the most important point: CHD is largely preventable.
Research from the Harvard School of Public Health shows that up to 80% of CHD cases could be prevented through lifestyle changes and early risk factor control. That means controlling:
Blood pressure
Cholesterol
Blood sugar
Weight
Smoking and alcohol consumption
Purpose of This Article
In this comprehensive guide, we will explore:
How the heart and coronary arteries work in health.
The risk factors for CHD (both controllable and uncontrollable).
The step-by-step biological process of how the disease develops.
Early warning signs and symptoms that should never be ignored.
Diagnostic tools doctors use to detect CHD.
Modern treatments and interventions, from medications to surgery.
Practical prevention strategies based on the latest research.
Our goal is to make this scientifically accurate yet easy to understand, so you can use this knowledge to protect your heart health — or help others protect theirs.
2 – The Anatomy and Function of the Heart and Coronary Arteries
Before we understand how coronary heart disease (CHD) develops, we must first know how a healthy heart works and why the coronary arteries are so crucial for life.
The Heart: A Life-Sustaining Pump
The human heart is a muscular organ roughly the size of your fist, located slightly to the left of the chest. It works like a tireless pump, contracting about 100,000 times a day to push blood through approximately 60,000 miles of blood vessels.
Right side of the heart: Pumps deoxygenated blood to the lungs, where it picks up oxygen.
Left side of the heart: Pumps oxygen-rich blood to the rest of the body.
This oxygenated blood is vital — without it, cells can’t produce the energy needed for survival.
The Coronary Circulation System
The heart itself is made of living muscle tissue (the myocardium), which also requires oxygen and nutrients. While blood flows through the chambers of the heart, this blood does not directly feed the heart muscle. Instead, the heart has its own dedicated network of blood vessels — the coronary arteries.
Main Coronary Arteries
Left Main Coronary Artery (LMCA) – Splits into:
Left Anterior Descending (LAD): Supplies the front of the heart.
Left Circumflex (LCX): Supplies the side and back of the heart.
Right Coronary Artery (RCA) – Supplies the right side and bottom of the heart, as well as part of the conduction system (which controls heartbeat rhythm).
These arteries are small — typically only 3–4 millimeters in diameter — but their role is critical. If any of them become blocked, even for minutes, the heart muscle they supply begins to die.
How Coronary Arteries Work
In a healthy artery:
The inner lining (endothelium) is smooth, allowing blood to flow freely.
The middle layer contains muscle that can expand or contract to adjust blood flow.
The outer layer provides strength and protection.
The coronary arteries adjust blood flow depending on the heart’s needs. For example, during exercise, they dilate to allow more oxygen-rich blood to reach the working heart muscle.
Why These Arteries Are Vulnerable
The coronary arteries are under constant pressure because the heart is always active. This makes them vulnerable to:
Damage from high blood pressure (hypertension).
Irritation from toxins in cigarette smoke.
Inflammation caused by high blood sugar in diabetes.
Cholesterol buildup from an unhealthy diet.
Once the endothelium is damaged, it becomes sticky, allowing cholesterol, calcium, and other substances to accumulate — the first step toward atherosclerosis.
The Heart’s Oxygen Demands
Even at rest, the heart consumes about 7–8% of the body’s total oxygen supply — more than many other organs. During stress or exercise, oxygen demand can triple. If the coronary arteries can’t meet this demand due to narrowing or blockage, symptoms like angina appear.
The Fragile Balance
A healthy coronary system is like a well-maintained highway — smooth, open, and able to handle traffic surges. CHD is like a slow-growing traffic jam caused by accidents (plaque formation) and roadblocks (blood clots). The earlier we understand this, the better we can prevent dangerous “traffic stoppages” that lead to heart attacks.
3 – How Coronary Heart Disease Develops: From Healthy Arteries to Dangerous Blockages
Coronary heart disease (CHD) does not happen overnight. It is the result of years or even decades of subtle changes in the coronary arteries. Understanding this step-by-step process is essential for prevention.
Step 1 – Endothelial Dysfunction (The First Crack in the Wall)
The endothelium, the thin layer of cells lining the inside of arteries, is like a protective Teflon coating — smooth, slippery, and resistant to clogs.
Damage factors include high blood pressure, smoking, high LDL cholesterol, high blood sugar, and chronic inflammation.
Once damaged, the endothelium becomes “sticky,” allowing substances in the blood to adhere to it.
Research from the Framingham Heart Study shows that endothelial dysfunction can start as early as teenage years in individuals with poor lifestyle habits.
Step 2 – Fatty Streak Formation
After the endothelium is damaged:
Low-Density Lipoprotein (LDL) cholesterol particles penetrate the artery wall.
The immune system detects these LDL particles as harmful and sends white blood cells (macrophages) to engulf them.
These macrophages, loaded with cholesterol, become foam cells — the earliest sign of plaque buildup.
These fatty streaks are not yet dangerous but set the stage for more severe changes. Autopsy studies have found fatty streaks in up to 50% of children in developed nations, showing how early the process can begin.
Step 3 – Plaque Growth (Atherosclerosis)
Over years, fatty streaks grow into atherosclerotic plaques composed of:
Cholesterol
Calcium
Cellular waste products
Fibrous tissue
The artery wall thickens, and the channel for blood flow narrows — a process called stenosis.
Mild stenosis: May cause no symptoms at rest.
Severe stenosis (>70% narrowing): Can trigger angina during exertion because blood flow cannot meet oxygen demand.
The American Heart Association reports that plaques can grow silently for decades before symptoms appear.
Step 4 – Plaque Instability and Rupture
Not all plaques are the same:
Stable plaques: Have a thick fibrous cap, grow slowly, and cause predictable symptoms.
Unstable plaques: Have a thin cap and a large lipid core. They can rupture suddenly, exposing the contents to the bloodstream.
When a plaque ruptures, the body treats it like a wound, activating clotting mechanisms. A blood clot (thrombus) forms, which can partially or completely block the coronary artery. This is the most common cause of heart attacks (myocardial infarctions).
Step 5 – Complete Blockage and Heart Muscle Death
If a coronary artery is completely blocked:
Blood supply to part of the heart stops.
Within minutes, heart muscle cells begin to die due to lack of oxygen (ischemia).
After about 20–40 minutes, irreversible damage begins — this is why immediate medical treatment is critical.
The Silent Nature of CHD
Many people assume CHD will give obvious warning signs, but that’s often not true:
Some individuals have silent ischemia, where blood flow is reduced but no pain is felt.
First symptom in many cases is a sudden heart attack.
According to the CDC, nearly 1 in 5 heart attack victims had no prior symptoms.
Inflammation: The Hidden Player
In the past, cholesterol was seen as the main villain. Now research shows that chronic inflammation is equally important in plaque formation and rupture.
High levels of C-reactive protein (CRP) in blood are linked to increased CHD risk.
Inflammation weakens plaque caps, making rupture more likely.
Key takeaway: CHD is a slow, complex process influenced by cholesterol, inflammation, genetics, and lifestyle. Prevention must start long before symptoms appear — ideally in childhood or early adulthood.
5 – Unmodifiable Risk Factors: What We Cannot Change but Must Understand
While many risk factors for coronary heart disease (CHD) can be reduced or eliminated through lifestyle changes, there are others that are beyond our control. Understanding these unmodifiable factors is still crucial — they help identify who is at higher risk and may require earlier or more aggressive preventive strategies.
1. Age
The risk of CHD increases significantly with age.
Men aged 45 and older and women aged 55 and older face a higher likelihood of developing symptoms.
Age-related changes in blood vessels, such as loss of elasticity and cumulative damage to the endothelium, make plaque formation more likely.
Scientific Insight:
A 2020 American College of Cardiology review noted that arterial stiffness increases by about 10% per decade after the age of 30, contributing to rising blood pressure and atherosclerosis risk.
2. Sex (Biological Differences)
Men generally develop CHD earlier than women, partly due to differences in hormones.
Estrogen in premenopausal women appears to protect against atherosclerosis by improving lipid profiles and maintaining vessel flexibility.
After menopause, women’s CHD risk catches up to — and may even surpass — that of men.
Important Note: Women often present with atypical symptoms (such as fatigue, nausea, or back pain) rather than the “classic” chest pain, which can delay diagnosis and treatment.
3. Genetics and Family History
A family history of premature CHD (before age 55 in men and 65 in women) significantly increases risk.
This can be due to inherited factors such as:
Familial hypercholesterolemia (extremely high LDL from birth)
Blood clotting disorders
Genetic variations affecting blood vessel repair
Research Highlight:
Studies have shown that having a parent with early CHD doubles a person’s risk, even after accounting for lifestyle.
4. Ethnicity and Ancestry
Some ethnic groups are at higher risk due to a combination of genetic predisposition, cultural dietary habits, and socioeconomic factors:
South Asians (India, Pakistan, Bangladesh, Sri Lanka): Higher rates of insulin resistance and metabolic syndrome, even at lower body weights.
African Americans: Higher prevalence of hypertension and obesity, both strong CHD drivers.
Hispanic/Latino populations: Elevated rates of diabetes, which accelerates atherosclerosis.
5. Existing Medical Conditions Present from Birth
Certain congenital heart defects or inherited metabolic disorders can increase lifetime CHD risk.
Examples:
Familial combined hyperlipidemia
Homocystinuria (a rare condition causing high homocysteine levels)
Why Understanding Unmodifiable Risk Matters
Even though these factors cannot be changed, they inform prevention strategy:
People with strong genetic or family history may need earlier cholesterol checks (sometimes in their 20s).
More aggressive control of modifiable risks (diet, exercise, blood pressure, and blood sugar) can offset inherited disadvantages.
Analogy: Think of unmodifiable risks as the cards you are dealt at birth — you cannot change them, but you can choose how to play them to avoid losing the game.
📌 Key Takeaway:
If you have unmodifiable risk factors, your focus should be on early detection and maximizing protective lifestyle habits. Medical monitoring may need to start years earlier than for someone without these risks.
6 – Modifiable Risk Factors: The Power to Change the Course of Coronary Heart Disease
Coronary heart disease (CHD) is not an inevitable fate. While some risk factors, such as age and genetics, are beyond human control, a significant number are modifiable — meaning that proactive lifestyle changes and medical interventions can greatly reduce the likelihood of developing the condition or slow its progression. Addressing these factors is not merely preventive medicine; it is an active step toward reshaping cardiovascular health.
1. Elevated Low-Density Lipoprotein (LDL) Cholesterol
The problem: LDL cholesterol is often labeled the “bad” cholesterol because it can infiltrate arterial walls, initiating inflammation and plaque formation (atherosclerosis).
Targets:
Optimal for healthy adults: <100 mg/dL
Optimal for high-risk patients: <70 mg/dL
Causes: Diets rich in saturated and trans fats, genetic conditions such as familial hypercholesterolemia, obesity, and inactivity.
Management:
Increase soluble fiber intake (oats, beans, apples).
Replace saturated fats with monounsaturated and polyunsaturated fats (olive oil, nuts, avocados).
If lifestyle changes fail, statins and other lipid-lowering agents may be prescribed.
Evidence: A 2019 Lancet meta-analysis confirmed that reducing LDL by 1 mmol/L (~39 mg/dL) cuts the risk of major vascular events by about 22%.
2. Hypertension (High Blood Pressure)
Why it matters: Persistently high blood pressure damages the endothelium, making arteries more vulnerable to cholesterol infiltration and plaque buildup.
Targets: <120/80 mmHg is ideal.
Causes: High sodium diets, obesity, stress, sedentary habits, and genetic predisposition.
Management:
Sodium restriction: Aim for <1,500 mg/day.
Dietary changes: Adopt the DASH diet.
Exercise: Minimum 150 minutes/week of moderate aerobic activity.
Stress reduction: Mindfulness or meditation practices.
Evidence: Data from the Framingham Heart Study indicates every 20 mmHg rise in systolic blood pressure doubles CHD mortality risk.
3. Tobacco Use
Impact: Chemicals in cigarette smoke damage vessel walls, accelerate plaque formation, and increase clotting tendency. Nicotine also raises heart rate and blood pressure.
Management:
Quit completely—“light” cigarettes or vaping are not safe alternatives.
Use nicotine replacement therapy or medications like varenicline if necessary.
Evidence: American Heart Association reports show CHD risk falls by 50% within one year of quitting and approaches that of a non-smoker within 15 years.
4. Poor Blood Sugar Control / Diabetes
Impact: High glucose damages blood vessels, promotes inflammation, and accelerates atherosclerosis.
Management:
Maintain HbA1c <7% (or as clinically indicated).
Follow a low-glycemic diet rich in whole foods.
Regular physical activity to improve insulin sensitivity.
Evidence: UKPDS research revealed each 1% drop in HbA1c lowers heart attack risk by 14%.
5. Physical Inactivity
Impact: Inactivity promotes obesity, insulin resistance, and hypertension.
Recommendation:
150 minutes/week of moderate-intensity exercise or 75 minutes/week vigorous exercise.
Incorporate daily movement: walking meetings, stair climbing, stretching breaks.
6. Unhealthy Diet
Risks: Diets high in processed foods, sugars, and unhealthy fats promote obesity, dyslipidemia, and inflammation.
Better options: Mediterranean, DASH, or plant-based diets.
Evidence: BMJ 2019 found adherence to the Mediterranean diet reduces CHD risk by up to 30%.
7. Excessive Alcohol
Risks: Raises blood pressure and triglycerides, promotes weight gain, and can cause cardiomyopathy.
Guidelines:
Women: ≤1 drink/day
Men: ≤2 drinks/day
For many, abstaining entirely is the safest choice.
8. Chronic Stress & Poor Sleep
Impact: Prolonged stress elevates cortisol, raising blood pressure and glucose. Inadequate sleep (<6 hours/night) increases CHD risk.
Management:
Relaxation practices: yoga, meditation, deep breathing.
Aim for 7–9 hours of quality sleep nightly.
Key Takeaway:
Modifiable risk factors are the most powerful lever in the fight against coronary heart disease. By addressing them early, individuals can reduce their CHD risk by more than half, even in the presence of genetic predispositions.
7 – Early Signs and Symptoms of Coronary Heart Disease: Recognizing the Silent Threat
Coronary heart disease (CHD) often develops silently over decades, with the early stages showing few — if any — obvious symptoms. This “quiet buildup” is why CHD is sometimes called the silent killer. However, the body often gives warning signals long before a heart attack occurs. Recognizing these early signs can lead to prompt medical evaluation, lifestyle changes, and treatment that may prevent catastrophic outcomes.
1. Angina Pectoris (Chest Discomfort)
Description: A sensation of pressure, heaviness, squeezing, or burning in the chest.
Pattern: Often triggered by physical exertion, emotional stress, or exposure to cold, and relieved by rest or nitroglycerin.
Types:
Stable angina: Predictable, occurs with exertion.
Unstable angina: New, worsening, or occurring at rest — a medical emergency.
Why it happens: Narrowed coronary arteries restrict blood flow, causing the heart muscle to demand more oxygen than is available.
Evidence: According to the American College of Cardiology, stable angina can precede a heart attack by months or years.
2. Shortness of Breath (Dyspnea)
Mechanism: Reduced oxygen delivery to the heart affects its pumping ability, leading to fluid buildup in the lungs.
When it occurs: May appear during exertion or even at rest in advanced disease.
Clues: Needing to stop frequently when walking or climbing stairs could indicate reduced cardiac reserve.
3. Fatigue and Reduced Exercise Tolerance
Description: Unusual tiredness, especially during activities that were previously easy.
Cause: The heart works harder to supply oxygen to the body, and diminished blood flow causes muscles to tire more quickly.
Clinical Insight: Particularly common in women, who may present with fatigue as a dominant symptom rather than chest pain.
4. Palpitations and Irregular Heartbeats
Reason: Ischemia can disrupt the heart’s electrical system, causing arrhythmias.
Warning: Sudden palpitations, especially with dizziness or fainting, warrant immediate medical evaluation.
5. Pain Beyond the Chest
CHD discomfort may radiate to:
Left arm (most common)
Jaw, neck, or back
Upper abdomen
Note: Pain patterns can differ by gender — women more often report neck, jaw, or back discomfort without classic chest pain.
6. Cold Sweats and Nausea
Mechanism: Reduced cardiac output triggers activation of the sympathetic nervous system, causing sweating, clamminess, and sometimes vomiting.
Significance: These symptoms, especially when paired with chest discomfort, are red flags for an impending heart attack.
7. Silent Ischemia
Definition: Episodes of reduced blood flow to the heart muscle without noticeable symptoms.
Risk groups: People with diabetes, the elderly, and those with previous heart damage.
Detection: Usually found through electrocardiogram (ECG) or stress testing.
When to Seek Immediate Medical Help
Call emergency services if you experience:
Chest pain or discomfort lasting more than a few minutes
Unexplained shortness of breath
Fainting, severe weakness, or sudden dizziness
Pain radiating to the arm, jaw, or back with sweating or nausea
Evidence: The National Heart, Lung, and Blood Institute warns that early treatment during the first “golden hour” of a heart attack can dramatically improve survival rates.
Key Takeaway:
CHD symptoms can range from obvious chest pain to vague fatigue or mild breathlessness. Because early detection greatly improves outcomes, it is critical not to ignore subtle or unusual changes in your body’s performance — particularly during physical activity.
8 – Diagnostic Methods for Coronary Heart Disease: From Clinical Clues to Definitive Tests
Identifying coronary heart disease (CHD) requires a careful blend of medical history, physical examination, and advanced diagnostic technology. Because CHD can hide behind subtle symptoms — or remain completely silent until a major event occurs — physicians often need multiple tools to confirm the diagnosis, assess severity, and guide treatment.
1. Detailed Medical History and Risk Assessment
A skilled physician begins with a thorough discussion of:
Symptoms: Type, frequency, duration, and triggers of chest discomfort, breathlessness, or fatigue.
Risk factors: Smoking, high blood pressure, diabetes, high cholesterol, family history of heart disease, sedentary lifestyle.
Lifestyle habits: Diet, exercise patterns, stress levels.
Why it matters: Understanding risk patterns helps the doctor decide which tests are most appropriate.
2. Physical Examination
Key aspects include:
Blood pressure measurement (to check for hypertension)
Heart and lung sounds (listening for murmurs, gallops, or fluid buildup)
Pulse checks (assessing rhythm and strength)
Signs of poor circulation (cold extremities, pale skin, leg swelling)
These findings alone cannot confirm CHD but can reveal clues about heart function.
3. Electrocardiogram (ECG or EKG)
Purpose: Measures the electrical activity of the heart.
What it shows: Past heart attacks, rhythm problems, and sometimes active ischemia.
Types:
Resting ECG: Done while you are still.
Exercise (stress) ECG: Performed during treadmill or stationary bike activity to detect exertion-induced ischemia.
Evidence: American Heart Association guidelines highlight ECG as a first-line test for suspected CHD.
4. Echocardiography (Heart Ultrasound)
Description: Uses sound waves to create images of the heart in motion.
Benefits:
Evaluates heart muscle movement.
Assesses valve function.
Detects areas of poor blood flow or previous damage.
Variants:
Stress echocardiography: Combines imaging with exercise or medication to reveal heart muscle weakness under strain.
5. Exercise Stress Testing
Purpose: Measures how well the heart performs under physical stress.
Method: Walking on a treadmill or cycling while connected to ECG, sometimes combined with imaging (nuclear or echo).
Significance: Can uncover ischemia that is not present at rest.
6. Nuclear Cardiology Imaging
Examples: SPECT or PET scans.
How it works: Radioactive tracers injected into the bloodstream reveal blood flow patterns in the heart muscle.
Value: Detects regions with poor perfusion, helping to differentiate between reversible ischemia and permanent damage.
7. Coronary Computed Tomography Angiography (CCTA)
Description: Advanced CT scan that visualizes coronary arteries in detail.
Advantages:
Non-invasive.
Can detect plaque buildup before major blockages form.
Use: Ideal for intermediate-risk patients to avoid unnecessary invasive procedures.
8. Cardiac Catheterization and Coronary Angiography
Gold standard for confirming CHD.
Procedure:
A catheter is inserted into a blood vessel (often in the wrist or groin) and guided to the coronary arteries.
Contrast dye highlights blockages on X-ray imaging.
Benefits: Allows immediate intervention (such as angioplasty) if a blockage is found.
Risks: Small risk of bleeding, infection, or artery damage.
9. Blood Tests
Cholesterol panel: Measures LDL (“bad”), HDL (“good”), and triglycerides.
Blood sugar & HbA1c: Screens for diabetes, a major CHD risk factor.
Cardiac enzymes: Troponin and CK-MB help detect recent heart muscle injury.
10. Emerging Technologies
Coronary artery calcium (CAC) scoring: Quantifies calcified plaque via CT scan.
Fractional flow reserve (FFR-CT): Uses computational modeling to assess blood flow significance of blockages.
Wearable devices: Smartwatches and patches that monitor heart rhythms and activity patterns.
Key Takeaway:
CHD diagnosis is not based on a single test but on a combination of history, examination, and targeted investigations. Early, accurate detection allows doctors to tailor treatments and prevent progression — often before irreversible heart damage occurs.
9 – Pathophysiology of Coronary Heart Disease: How Arteries Narrow and Heart Attacks Happen
Coronary heart disease (CHD) is not a sudden event—it is the result of a slow, complex process inside the walls of the coronary arteries. This process, called atherosclerosis, begins silently years before symptoms appear. Understanding how it develops is key to understanding how to prevent and treat CHD.
1. The Endothelium: The Heart’s Protective Lining
The endothelium is a thin layer of cells lining the inside of every blood vessel.
It produces substances that:
Keep blood flowing smoothly.
Prevent clot formation.
Control the opening and narrowing of the arteries.
Damage to the endothelium is the first step toward CHD.
Causes of damage:
High LDL cholesterol.
High blood pressure.
Smoking chemicals.
High blood sugar from diabetes.
Chronic inflammation.
2. The Role of LDL Cholesterol
LDL (low-density lipoprotein) is often called “bad cholesterol” because when too much circulates in the blood, it can enter damaged areas of the endothelium.
Once inside, LDL particles become oxidized—a chemical change that triggers the immune system.
3. Inflammation and Immune Response
The immune system mistakes oxidized LDL as harmful.
White blood cells (macrophages) rush to the area to “swallow” the LDL.
These cells become foam cells, forming the earliest visible signs of atherosclerosis called fatty streaks.
4. Plaque Formation
Over time:
Foam cells accumulate.
Smooth muscle cells from deeper artery layers migrate toward the inner wall.
These cells produce fibrous tissue, creating a plaque that bulges into the artery space.
Plaque composition:
Core: Cholesterol, dead cells, waste products.
Cap: A layer of fibrous tissue covering the core.
5. Artery Narrowing (Stenosis)
As plaque grows, it reduces the space for blood to flow.
This narrowing is called stenosis.
At rest, the heart may still receive enough blood.
During exercise or stress, reduced blood flow can cause angina (chest pain).
6. Plaque Rupture and Clot Formation
Not all plaques are stable.
Vulnerable plaques have thin fibrous caps and large lipid cores.
If a plaque ruptures:
Blood is exposed to the plaque’s contents.
This triggers platelet activation and a clot (thrombus) forms.
The clot can partially or completely block blood flow.
7. Heart Attack (Myocardial Infarction)
If a clot blocks blood flow completely, the heart muscle downstream is deprived of oxygen.
Within minutes, cells start to die—a myocardial infarction.
The size and location of the blockage determine the severity of the damage.
8. Microvascular Dysfunction
Not all CHD is caused by large-artery blockages.
Sometimes, the small vessels (microcirculation) supplying the heart fail to dilate properly.
This condition—microvascular angina—can cause chest pain even when large arteries appear normal on angiography.
9. The Role of Systemic Inflammation
Atherosclerosis is now recognized as an inflammatory disease as much as a cholesterol problem.
Chronic inflammation:
Weakens plaques.
Makes rupture more likely.
This explains why infections, autoimmune conditions, and chronic stress can influence heart disease risk.
10. The Silent Progression
CHD can progress without noticeable symptoms for decades.
The first sign in some people is sudden cardiac death.
This is why screening and early detection are critical for at-risk individuals.
Key Takeaway:
Coronary heart disease develops through endothelial injury, lipid buildup, inflammation, and plaque growth. A sudden rupture and clot formation can lead to heart attack. Understanding this chain of events is crucial for both prevention and treatment strategies.
10 – Risk Factors for Coronary Heart Disease: What We Can and Cannot Change
Coronary heart disease (CHD) does not develop randomly—it is strongly linked to risk factors that either can be changed (modifiable) or cannot be changed (non-modifiable). Understanding both types is essential for designing effective prevention strategies.
1. Modifiable Risk Factors
These are lifestyle or health conditions that you can influence through changes in behavior, medical treatment, or both.
a. High LDL Cholesterol
Why it matters: Excess LDL cholesterol promotes plaque buildup in arteries.
Prevention and control:
Diet rich in fruits, vegetables, and whole grains.
Limiting saturated and trans fats.
Regular physical activity.
Statins or other lipid-lowering medications if needed.
b. High Blood Pressure (Hypertension)
Why it matters: High pressure damages the endothelium, making it easier for cholesterol to enter the artery wall.
Control strategies:
Reduce sodium intake.
Increase potassium-rich foods.
Regular exercise.
Antihypertensive medications when necessary.
c. Smoking
Why it matters: Chemicals in tobacco cause direct endothelial injury and increase clot formation.
Benefits of quitting:
Heart attack risk drops by 50% within a year.
Circulation and lung function improve quickly.
d. Physical Inactivity
Why it matters: Sedentary living reduces “good” HDL cholesterol, increases obesity risk, and impairs vascular health.
Recommendation: At least 150 minutes of moderate aerobic exercise per week.
e. Unhealthy Diet
Why it matters: Diets high in processed foods, added sugars, and saturated fats accelerate atherosclerosis.
Better choice: The Mediterranean diet, DASH diet, or plant-based eating.
f. Overweight and Obesity
Why it matters: Excess fat, especially abdominal fat, is linked to insulin resistance, high blood pressure, and dyslipidemia.
Goal: Even a 5–10% weight loss can significantly improve heart health.
g. Diabetes and Prediabetes
Why it matters: High blood sugar damages blood vessels and promotes inflammation.
Management: Blood sugar control through diet, exercise, and medication.
h. Chronic Stress
Why it matters: Long-term stress raises cortisol and adrenaline, increasing blood pressure and inflammation.
Control: Stress management techniques like meditation, deep breathing, and adequate sleep.
i. Excessive Alcohol Consumption
Why it matters: Heavy drinking raises blood pressure and triglycerides.
Safe limits: Up to one drink per day for women, two for men.
2. Non-Modifiable Risk Factors
These cannot be changed, but knowing them helps identify who needs more aggressive prevention.
a. Age
Risk rises sharply after:
Men: 45 years old.
Women: 55 years old or after menopause.
b. Sex
Men generally develop CHD earlier than women.
Women’s risk increases after menopause due to decreased estrogen protection.
c. Family History
Having a first-degree relative (parent, sibling) with early CHD increases risk:
Men: before age 55.
Women: before age 65.
d. Genetic Disorders
Conditions like familial hypercholesterolemia cause extremely high cholesterol from birth.
3. Emerging and Less-Recognized Risk Factors
Chronic inflammatory diseases (e.g., rheumatoid arthritis, lupus).
Sleep disorders (sleep apnea).
Air pollution exposure.
High lipoprotein(a) levels—an inherited cholesterol particle linked to higher risk.
4. The Risk Factor Multiplier Effect
Having multiple risk factors multiplies—not just adds—the total risk.
Example: Smoking + high blood pressure + high cholesterol can make the risk 10 times higher than having one risk factor alone.
Key Takeaway:
While you can’t change your age, sex, or genes, most major risk factors for CHD are preventable or manageable. The earlier these are addressed, the lower the lifetime risk of heart disease.
11 – Early Warning Signs and Symptoms of Coronary Heart Disease
Coronary heart disease (CHD) often develops silently over decades, which means symptoms may be absent in the early stages. However, as plaque builds up and blood flow to the heart is reduced, the body begins to send warning signals. Recognizing these early signs can be life-saving.
1. The Silent Phase
In its initial stage, CHD may progress without noticeable symptoms. This is why it is sometimes called the “silent killer”—damage occurs inside the arteries long before pain or discomfort is felt.
People with risk factors (high cholesterol, high blood pressure, smoking, diabetes) are most vulnerable.
A routine medical check-up may reveal early clues: abnormal cholesterol levels, elevated blood pressure, or signs of heart strain on an ECG.
2. Angina Pectoris (Chest Pain or Discomfort)
The most classic symptom of CHD is angina—a squeezing, pressure-like, or burning discomfort in the chest caused by reduced blood flow to the heart muscle.
Typical Angina Characteristics:
Location: Usually behind the breastbone, sometimes radiating to the neck, jaw, shoulders, or arms (especially the left arm).
Triggers: Physical exertion, emotional stress, cold weather, or heavy meals.
Duration: Usually lasts a few minutes and improves with rest or nitroglycerin.
Sensation: Described as pressure, heaviness, or tightness rather than sharp pain.
Stable vs. Unstable Angina:
Stable Angina: Predictable pattern, occurs during activity, relieved by rest.
Unstable Angina: Sudden onset, occurs even at rest, lasts longer, and signals a high risk of heart attack—a medical emergency.
3. Shortness of Breath (Dyspnea)
When the heart cannot pump efficiently, oxygen delivery to the body drops. This may cause:
Breathlessness during activity (early stage).
Breathlessness even while resting (advanced stage).
Worsening at night or when lying flat.
4. Fatigue and Reduced Exercise Tolerance
People with developing CHD may feel unusually tired during activities that previously felt easy.
This fatigue can be subtle and gradual, often mistaken for aging or lack of fitness.
5. Palpitations or Irregular Heartbeat
Reduced blood flow and oxygen can irritate the heart’s electrical system, causing skipped beats or rapid rhythms.
In some cases, arrhythmias may be the first noticeable sign of CHD.
6. Dizziness or Fainting (Syncope)
Severe narrowing of coronary arteries may cause transient drops in blood pressure, leading to lightheadedness or fainting.
7. Symptoms in Women: Often Atypical
Women may experience different warning signs than men, which can delay diagnosis:
Discomfort in the back, neck, or jaw.
Nausea, vomiting, or indigestion-like pain.
Unusual fatigue lasting days.
Shortness of breath without chest pain.
8. Silent Myocardial Ischemia
Some individuals, especially those with diabetes, may have silent episodes of reduced blood flow to the heart muscle without any pain or discomfort.
Detected only during tests like ECG or stress testing.
Dangerous because it can lead to a heart attack without prior warning.
9. When Symptoms Signal a Heart Attack
Immediate emergency attention is needed if you experience:
Severe chest pressure lasting more than a few minutes.
Pain spreading to the arm, neck, or jaw.
Profuse sweating, nausea, or a feeling of impending doom.
Shortness of breath at rest.
Key Takeaway:
CHD symptoms can range from barely noticeable fatigue to life-threatening chest pain. Being aware of both typical and atypical signs—especially in high-risk individuals—can lead to early diagnosis, better treatment outcomes, and reduced risk of sudden cardiac death.
12 – How Coronary Heart Disease is Diagnosed: Modern Tests and Tools
Diagnosing Coronary Heart Disease (CHD) requires a combination of medical history, physical examination, and advanced diagnostic tests. The goal is to detect the condition early, determine its severity, and guide the best treatment plan before serious complications occur.
1. Step One – Medical History and Risk Assessment
The first step in diagnosis is a thorough patient interview. The doctor will:
Ask about symptoms (chest pain, shortness of breath, fatigue).
Review risk factors (smoking, high cholesterol, diabetes, family history).
Explore lifestyle habits (diet, exercise, stress).
Note any previous heart issues or hospital visits.
Why it matters:
A detailed history helps the doctor estimate the probability of CHD even before tests are done.
2. Step Two – Physical Examination
A hands-on assessment includes:
Measuring blood pressure and heart rate.
Listening to the heart for murmurs or irregular rhythms.
Checking for swelling in the legs (possible sign of heart failure).
Looking for skin changes (pale or bluish color due to poor circulation).
3. Laboratory Blood Tests
Blood work can reveal clues about heart health:
Lipid profile – measures cholesterol and triglycerides.
Blood glucose & HbA1c – detects diabetes, a major CHD risk factor.
High-sensitivity C-reactive protein (hs-CRP) – measures inflammation in arteries.
Troponin – a marker of heart muscle damage (used in suspected heart attacks).
4. Electrocardiogram (ECG or EKG)
A quick, painless test that records the heart’s electrical activity:
Detects irregular heart rhythms (arrhythmias).
Shows signs of past or ongoing heart attacks.
May reveal silent ischemia (reduced blood flow without symptoms).
5. Exercise Stress Test (Treadmill Test)
The patient walks on a treadmill or pedals a stationary bike while hooked to an ECG:
Measures how the heart responds to physical exertion.
Helps detect blockages that only cause problems during activity.
Variations: Pharmacologic stress test (for patients unable to exercise).
6. Echocardiogram (Heart Ultrasound)
Uses sound waves to create moving images of the heart:
Assesses heart muscle function and pumping efficiency.
Detects valve problems, wall motion abnormalities, and damage from past heart attacks.
7. Stress Echocardiogram
Combines an echocardiogram with exercise or medication-induced stress:
Highlights parts of the heart that don’t get enough blood during exertion.
8. Nuclear Stress Test (Myocardial Perfusion Imaging)
Involves injecting a small amount of radioactive tracer into the bloodstream.
A special camera detects areas of the heart that receive less blood flow.
Provides highly accurate mapping of blockages.
9. Coronary Calcium Scan (CT Calcium Scoring)
A CT scan measures calcium deposits in coronary arteries.
Higher calcium scores indicate greater plaque buildup and higher CHD risk.
Useful for early detection in asymptomatic individuals.
10. Coronary CT Angiography (CTA)
A non-invasive imaging test:
Uses contrast dye and CT scanning to visualize coronary arteries in detail.
Detects narrowing or blockages without the need for catheterization.
11. Cardiac Catheterization & Coronary Angiography
The gold standard for diagnosing CHD:
A catheter is inserted through an artery in the wrist or groin.
Contrast dye is injected, and X-ray images show the exact location and severity of blockages.
Allows for immediate treatment, such as angioplasty or stent placement.
12. Additional Functional Tests
In selected patients:
Cardiac MRI – provides detailed images of heart structure and function.
Intravascular Ultrasound (IVUS) – a tiny ultrasound probe inside the artery for microscopic plaque imaging.
Fractional Flow Reserve (FFR) – measures pressure differences to determine how severely a blockage is restricting blood flow.
Key Takeaway:
There is no one-size-fits-all diagnostic approach. Doctors choose tests based on the patient’s symptoms, risk level, and overall health. Early detection is critical because CHD often remains silent until it causes major, sometimes irreversible, damage.
13 – Treatment Options for Coronary Heart Disease: From Lifestyle Changes to Advanced Cardiac Procedures
Coronary Heart Disease (CHD) is a manageable condition, and with the right approach, many people live long, active lives. The treatment strategy depends on how advanced the disease is, the severity of symptoms, and the patient’s overall health. Treatment aims to:
Improve blood flow to the heart.
Relieve symptoms like chest pain and shortness of breath.
Prevent heart attacks and further damage.
Slow or reverse disease progression.
1. Lifestyle Modifications – The Foundation of CHD Management
Before any pills or procedures, doctors emphasize changing daily habits to improve heart health.
Healthy Diet
Focus on whole foods: fruits, vegetables, whole grains, legumes, nuts, and seeds.
Limit saturated and trans fats, red meat, processed snacks, and sugary drinks.
Reduce sodium intake to help lower blood pressure.
Follow evidence-based patterns like the Mediterranean diet or DASH diet.
Regular Physical Activity
Aim for 150 minutes per week of moderate aerobic exercise (e.g., brisk walking, cycling, swimming).
Include muscle-strengthening activities at least twice weekly.
Always consult a doctor before starting if you have advanced CHD.
Weight Management
Achieve and maintain a healthy body mass index (BMI).
Even a modest weight loss of 5–10% can significantly improve blood pressure, cholesterol, and blood sugar.
Smoking Cessation
Quitting smoking immediately reduces CHD risk—benefits start within weeks.
Use nicotine replacement therapy, prescription medications, or support groups if needed.
Stress Reduction
Chronic stress can worsen CHD by increasing inflammation and blood pressure.
Practices like yoga, meditation, deep breathing, or tai chi are beneficial.
2. Medications – Controlling Risk Factors and Symptoms
When lifestyle changes alone aren’t enough, medications play a crucial role.
Antiplatelet Agents
Example: Aspirin or Clopidogrel.
Prevent platelets from clumping and forming blood clots.
Cholesterol-Lowering Drugs
Statins (e.g., atorvastatin, rosuvastatin) reduce LDL cholesterol and stabilize plaques.
Ezetimibe or PCSK9 inhibitors for patients who don’t respond well to statins.
Blood Pressure Medications
Beta-blockers – reduce heart rate and blood pressure, lowering oxygen demand.
ACE inhibitors or ARBs – relax blood vessels and reduce heart strain.
Calcium channel blockers – widen arteries and improve blood flow.
Nitrates
Example: Nitroglycerin.
Quickly relieve chest pain (angina) by dilating coronary arteries.
Diabetes Medications
Controlling blood sugar helps prevent plaque buildup and artery damage.
3. Interventional Procedures – Restoring Blood Flow
If blockages are severe or symptoms persist despite medication, doctors may recommend minimally invasive procedures.
Percutaneous Coronary Intervention (PCI)
Also called angioplasty.
A balloon-tipped catheter is inserted to widen narrowed arteries.
Usually followed by stent placement to keep the artery open.
Drug-Eluting Stents
Coated with medication that prevents scar tissue formation.
Reduces the risk of re-narrowing.
4. Surgical Options – For Extensive Disease
For multiple or severe blockages, open-heart surgery may be necessary.
Coronary Artery Bypass Grafting (CABG)
Surgeons create a new path for blood to reach the heart by grafting blood vessels from the leg, arm, or chest.
Preferred for patients with multiple blockages or diabetes.
5. Cardiac Rehabilitation – The Recovery and Prevention Program
After a heart attack, surgery, or diagnosis, many patients benefit from cardiac rehab:
Supervised exercise training.
Nutrition and lifestyle counseling.
Emotional support and stress management.
Key Takeaway
Managing CHD is not just about reacting to symptoms—it’s about building a long-term strategy that combines lifestyle, medication, and medical interventions when needed. The earlier treatment starts, the greater the chance of preventing heart attacks and improving quality of life.
14 – Preventing Coronary Heart Disease: Science-Backed Strategies for a Healthy Heart
While modern medicine offers effective treatments for Coronary Heart Disease (CHD), prevention remains the most powerful tool. Many risk factors for CHD are modifiable, meaning you can take action to significantly reduce your chances of developing the condition—sometimes by over 80% according to large epidemiological studies.
1. Understanding the Prevention Mindset
Prevention is not a single action—it’s a lifelong commitment to maintaining heart health. Think of it as building a “shield” around your arteries to protect them from damage and plaque buildup. This shield is formed through daily habits, medical checkups, and an awareness of your own risk profile.
2. Primary vs. Secondary Prevention
Primary Prevention: Steps taken to avoid developing CHD in the first place.
Secondary Prevention: Measures to prevent the worsening of CHD or recurrence of events in those already diagnosed.
Both require similar lifestyle strategies, but secondary prevention is more aggressive and often includes medical treatment.
3. Core Lifestyle Strategies for CHD Prevention
A. Eat for Your Arteries
A healthy diet is one of the strongest weapons against CHD:
Increase: Vegetables, fruits, legumes, nuts, seeds, whole grains, fatty fish (rich in omega-3 fatty acids).
Reduce: Processed meats, sugary drinks, fried foods, foods high in trans fats and refined carbohydrates.
Follow proven patterns: The Mediterranean diet, DASH diet, or Portfolio diet have been shown to improve cholesterol, blood pressure, and inflammation.
B. Stay Physically Active
The heart thrives on movement:
Aim for 150 minutes of moderate-intensity aerobic activity (like brisk walking or cycling) per week.
Add muscle-strengthening exercises twice weekly.
Even short bursts of activity throughout the day—like taking the stairs—help reduce risk.
C. Maintain a Healthy Weight
Excess body fat, especially around the waist, increases risk of high cholesterol, high blood pressure, and insulin resistance.
Target a Body Mass Index (BMI) between 18.5 and 24.9, and keep waist circumference under:
40 inches (102 cm) for men.
35 inches (88 cm) for women.
D. Avoid Tobacco Completely
Smoking damages arteries, reduces oxygen delivery, and accelerates plaque buildup.
Quitting smoking immediately reduces CHD risk and continues to bring benefits over the years.
Even secondhand smoke is harmful—avoid exposure.
E. Manage Stress
Chronic stress triggers inflammatory and hormonal changes that harm the cardiovascular system.
Use techniques like mindfulness, meditation, yoga, deep breathing, or regular hobbies.
Build a supportive social network—loneliness and isolation can also raise heart risk.
4. Regular Health Monitoring
Prevention is not guesswork—it’s tracking and adjusting:
Blood Pressure: Maintain under 120/80 mmHg.
Cholesterol: LDL (“bad” cholesterol) as low as possible; HDL (“good” cholesterol) higher is better.
Blood Sugar: Fasting glucose under 100 mg/dL; HbA1c under 5.7%.
Get regular screenings starting in your 20s, or earlier if you have a family history of heart disease.
5. Preventing CHD in Special Groups
People with Diabetes
Keep blood sugar strictly controlled.
Choose low-glycemic index foods.
Monitor blood pressure and cholesterol more frequently.
Women
Be aware that heart disease is the leading cause of death in women—symptoms can be subtler.
Hormonal changes during menopause can raise cholesterol and blood pressure.
Older Adults
Prevention still works at any age—diet, activity, and medication compliance are crucial.
6. The Role of Medical Support in Prevention
Work with your healthcare provider to assess 10-year and lifetime CHD risk.
If risk is high, preventive medications like statins or low-dose aspirin may be prescribed.
Participate in preventive programs like cardiac screenings or community heart health workshops.
7. Key Takeaway
Preventing CHD is a proactive journey, not a one-time fix. Every healthy choice you make today—what you eat, how you move, how you manage stress—helps protect your arteries tomorrow. Prevention is both the cheapest and most effective “treatment” for heart disease.
15 – The Global Impact of Coronary Heart Disease and the Future of Prevention
Coronary Heart Disease (CHD) is not just a personal health concern—it is a global health crisis. Its burden extends beyond the lives it claims, affecting economies, healthcare systems, and communities. Understanding its worldwide impact helps us see why prevention and innovation are urgent priorities.
1. CHD as the World’s Leading Killer
According to the World Health Organization (WHO):
CHD is responsible for approximately 17.9 million deaths each year, representing about one-third of all global deaths.
Of these, over 85% are due to heart attacks and strokes, the majority linked to atherosclerosis.
More than three-quarters of CHD deaths occur in low- and middle-income countries, where prevention and treatment resources are often limited.
2. The Economic Toll
CHD is costly in multiple ways:
Direct healthcare costs: Hospitalizations, surgeries, medications, and long-term care.
Indirect costs: Loss of productivity, early retirement, and disability.
In the United States alone, CHD costs exceed $200 billion annually, and projections suggest this will rise dramatically without stronger prevention programs.
3. Global Disparities in CHD Burden
Not all regions experience CHD in the same way:
High-income countries have seen declining CHD mortality rates over the past 40 years—largely due to public health campaigns, better medical treatments, and lifestyle changes.
Developing nations are facing a CHD surge, fueled by urbanization, poor diet, smoking, and lack of access to healthcare.
Many rural and underserved populations have limited access to preventive screenings, leading to late diagnoses.
4. The Role of Urbanization and Globalization
Global lifestyle shifts are influencing CHD risk:
Increased consumption of processed, high-calorie foods.
Reduced physical activity due to more sedentary jobs.
Higher stress levels linked to rapid economic and social changes.
Exposure to air pollution, which has been shown to increase the risk of heart attacks.
5. Current Global Strategies to Combat CHD
Efforts to reduce the burden of CHD include:
WHO’s “Global Hearts” Initiative: Focuses on reducing salt intake, controlling blood pressure, and improving tobacco control.
Public Health Policies: Implementing sugar taxes, banning trans fats, and mandating food labeling.
Community-Based Programs: Local exercise groups, cooking classes, and free health screenings.
6. Future Directions in CHD Prevention and Treatment
Emerging research and technology hold promise for dramatically reducing CHD:
Precision Medicine: Tailoring prevention and treatment based on genetic profiles.
Wearable Health Technology: Devices that track heart rate, detect irregular rhythms, and even alert for early heart attack signs.
AI-Powered Diagnostics: Early detection of CHD using advanced imaging and big data analysis.
Regenerative Medicine: Stem cell therapies aimed at repairing damaged heart tissue.
Plant-Based Pharmaceuticals: Exploring compounds in plants for cholesterol reduction and anti-inflammatory effects.
7. A Vision for a CHD-Free Future
To significantly reduce CHD’s global toll, we must:
Strengthen public education about heart health from childhood.
Ensure universal access to basic healthcare and preventive screenings.
Invest in clean environments, healthy food systems, and safe spaces for physical activity.
Support international collaborations between governments, NGOs, and the private sector.
8. Key Takeaway
CHD’s global impact is both a warning and an opportunity. While it remains the leading cause of death worldwide, we have powerful tools—scientific knowledge, proven prevention strategies, and emerging technologies—to turn the tide. The challenge is not just medical—it’s political, economic, and societal. With coordinated global action, CHD could one day be as rare as diseases that have been nearly eradicated through human effort.
16 – Conclusion and Practical Takeaways for Readers
Coronary Heart Disease (CHD) is often called a silent killer—it can develop quietly over decades, only revealing itself in the form of a heart attack, angina, or sudden cardiac death. But this does not mean CHD is inevitable. The overwhelming evidence shows that with the right knowledge, timely action, and consistent lifestyle habits, the majority of CHD cases are preventable.
1. The Big Picture
CHD develops through a complex interaction of genetics, lifestyle, and environmental factors.
Risk factors such as high blood pressure, high LDL cholesterol, smoking, obesity, diabetes, and chronic stress often work together to accelerate atherosclerosis.
Early prevention is more effective than late treatment. Every year of healthy living adds protection against arterial damage.
2. What Science Has Taught Us
Diet matters: Diets rich in fruits, vegetables, whole grains, lean proteins, and healthy fats protect arteries, while diets high in sugar, trans fats, and processed foods promote plaque buildup.
Movement is medicine: Regular exercise strengthens the heart muscle, improves circulation, and lowers multiple CHD risk factors.
Stress management is not optional: Chronic stress increases blood pressure and inflammatory processes that harm the heart.
Early detection saves lives: Simple tests—like blood pressure checks, cholesterol panels, and fasting glucose—can identify risks long before symptoms appear.
3. Practical Daily Actions to Protect Your Heart
Nutrition
Limit salt to <2,300 mg/day (about 1 teaspoon).
Aim for 25–30 grams of fiber daily.
Reduce intake of ultra-processed foods and sugary drinks.
Physical Activity
Target 150 minutes of moderate-intensity exercise per week (e.g., brisk walking, cycling, swimming).
Include strength training twice weekly.
Lifestyle
Quit smoking and avoid secondhand smoke entirely.
Maintain a healthy weight and waist circumference.
Practice daily stress-reducing activities like meditation, deep breathing, or yoga.
Medical Care
Monitor blood pressure, cholesterol, and glucose annually (or more often if at risk).
Follow prescribed medications exactly as directed.
Discuss family history with your doctor—especially if a parent or sibling had early heart disease.
4. Mindset for Lifelong Heart Health
Protecting your heart is not a one-time project—it’s a lifelong partnership with your own body. This means:
Thinking of healthy choices as investments, not restrictions.
Celebrating small wins: Every healthier meal, every walk, every skipped cigarette counts.
Staying informed: Medical science evolves, and new prevention tools are emerging every year.
5. The Hope for the Future
We stand at a point where CHD could shift from being the world’s number one killer to a largely preventable condition. Through:
Better global education
Affordable healthcare access
Smarter public policies
Innovative medical technology
…the world could see a massive decline in heart-related deaths within a single generation.
Final Thought
Your heart beats about 100,000 times a day—without pause, without rest. The least we can do is give it the care it needs to keep beating strong for decades to come.
Every step you take toward prevention—no matter how small—puts you on the side of health, vitality, and longevity. Start today, because your heart’s future begins with the choices you make now.