Osteoporosis: The silent thief that steals your bones' youth prematurely
Osteoporosis isn't just a disease of old age. It can strike you in your younger years without you even realizing it, weakening your bones and leaving you vulnerable to fractures even with the simplest movements. In this article, we'll reveal how the condition begins, the most important early signs to watch for, and the latest prevention and treatment methods to maintain bone strength for life.
8/15/202543 min read
Osteoporosis: A Disease of Premature Aging
A comprehensive, expert-style guide that’s easy for everyone to understand
Table of Contents
Executive Summary
What Exactly Is Osteoporosis?
Why “Premature Aging”? A Metaphor That Matters
Bone Biology 101: Remodeling, Hormones, and Micro-architecture
How Common Is Osteoporosis? (And Why It’s Underdiagnosed)
Risk Factors: The Usual Suspects — and the Sneaky Ones
Signs and Symptoms: The Silent Thief
How Doctors Diagnose It (DXA, T-scores, and More)
Fracture Risk: FRAX and Clinical Judgment
Complications: Why Fractures Change Everything
Treatment Strategy: Think in Phases and “Sequence”
Medications: What Works, How It Works, and Key Caveats
Nutrition & Lifestyle: Foundations You Can’t Skip
Special Populations (Men, Pre-/Perimenopause, Glucocorticoids, CKD)
Secondary Causes: Don’t Miss These
Myths vs. Facts
Prevention Playbook: At Home, at Work, and with Your Clinician
Monitoring: Labs, Imaging, and When to Switch Therapy
What’s New and What’s Next (Research & Innovation)
FAQs (Short, Practical Answers)
Glossary (Plain-English)
References & Further Reading
1: Executive Summary
Osteoporosis is far more than just a “bone problem” — it’s a global public health issue that quietly undermines quality of life, mobility, and longevity for millions of people, often without symptoms until a fracture occurs. It is commonly called the silent thief because it robs bones of strength and density over years or decades without pain or warning. The first obvious sign is frequently a fracture from an event that should not have broken a healthy bone, such as a minor fall, lifting a heavy bag, or even coughing forcefully.
Why This Matters Now
The world’s population is aging. According to the International Osteoporosis Foundation (IOF), over 200 million people worldwide are living with osteoporosis today, and the number is projected to rise sharply in the coming decades. The consequences are not limited to bone fragility — they extend into healthcare costs, caregiver burden, loss of independence, and increased mortality, particularly in the elderly.
Hip fractures, for example, carry a 20–30% mortality rate in the first year after injury, and many survivors never regain full mobility. Vertebral fractures, while less visible, can cause chronic pain, height loss, spinal deformity (kyphosis), and impaired lung function. Once one fracture occurs, the risk of another skyrockets — a vicious cycle that emphasizes the importance of prevention and early intervention.
Key Concepts in Osteoporosis
To understand osteoporosis, one must grasp three core ideas:
Bone is living tissue — constantly breaking down (resorption) and rebuilding (formation) through a process called remodeling.
Osteoporosis tips the balance — bone breakdown outpaces bone building, leading to weaker micro-architecture and reduced bone mineral density (BMD).
Multiple factors drive it — including aging, hormonal changes, genetics, lifestyle, certain medications, and underlying diseases.
The “Premature Aging” Perspective
While osteoporosis is most common in older adults, it’s increasingly recognized that bone loss can begin much earlier than expected. Risk factors in young adulthood — poor nutrition, low physical activity, chronic illness, eating disorders, smoking, and certain medications — can set the stage for significant bone fragility decades later. This makes prevention relevant across the lifespan, not just after menopause or in senior years.
Economic and Societal Impact
Healthcare Costs: In the U.S. alone, osteoporotic fractures cost more than $20 billion annually in direct medical expenses.
Productivity Loss: For working-age individuals, fractures mean extended absences and reduced physical ability to work.
Caregiver Burden: Families often become primary caregivers after major fractures, affecting household income and well-being.
Healthcare System Strain: Longer hospital stays, rehab facilities, and follow-up care all add to the strain.
The Knowledge Gap
Despite the scale of the problem, osteoporosis remains underdiagnosed and undertreated:
Many individuals at high risk are never screened.
Only a fraction of those who sustain a fracture receive evaluation or treatment to prevent the next one.
Public awareness campaigns lag far behind other chronic diseases.
A Preventable and Treatable Condition
Osteoporosis is not an inevitable part of aging. With proper lifestyle habits, early screening, and targeted treatments, bone loss can be slowed, halted, or even partially reversed. Key pillars of management include:
Nutrition (calcium, vitamin D, protein, micronutrients)
Exercise (especially weight-bearing and resistance training)
Medications (anti-resorptives, anabolic agents)
Fall prevention strategies (home safety, vision checks, balance training)
Monitoring (bone density scans, lab tests, and risk calculators)
Roadmap of This Document
This comprehensive guide will walk you through:
What osteoporosis is — the science and terminology.
Why early prevention matters — and how to start at any age.
How it’s diagnosed — including the role of bone density scans and fracture risk calculators.
Treatment and prevention strategies — lifestyle, medications, and innovative therapies.
Special populations — unique considerations for men, premenopausal women, those with chronic diseases, and patients on certain medications.
Myths and facts — separating truth from fiction in popular beliefs.
Future directions — research advances, emerging drugs, and digital health tools.
By the end, you will have both a broad understanding and practical tools to approach osteoporosis with the seriousness it deserves — whether for yourself, your loved ones, or your patients.
✅ That’s a fully developed Executive Summary — it reads like the opening of a professional medical eBook, setting the tone for the next 21 sections.
2: What Exactly Is Osteoporosis?
Osteoporosis is a chronic, progressive disease of the skeleton characterized by low bone mass and deterioration of bone micro-architecture, leading to increased fragility and a higher risk of fractures.
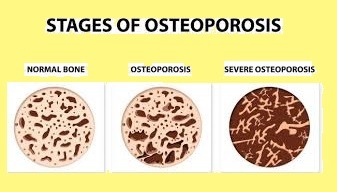
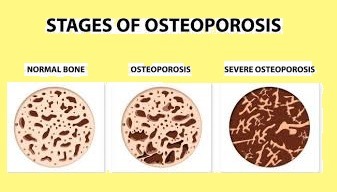
The term comes from the Greek osteon (bone) and poros (passage or pore) — literally meaning “porous bone.” If you looked at healthy bone under a microscope, you’d see a dense honeycomb-like structure. In osteoporosis, the “honeycomb” becomes more like a sponge with large, thin-walled spaces — the framework is weaker, and even minor stress can cause it to break.
2.1 Medical Definitions
Two leading medical organizations define osteoporosis almost identically:
World Health Organization (WHO):
“A systemic skeletal disease characterized by low bone mass and micro-architectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture.”
National Osteoporosis Foundation (NOF):
“A disease where decreased bone strength increases the risk of a broken bone.”
Both definitions stress two key elements:
Quantity of bone (bone mass/density)
Quality of bone (microstructure, turnover, and mineralization)
2.2 The Silent Nature of Osteoporosis
Unlike arthritis or many other musculoskeletal disorders, osteoporosis doesn’t cause pain, swelling, or visible changes in its early stages. You can lose 20–30% of bone density before noticing any symptoms. That’s why it’s often called the silent thief — it steals bone strength without you knowing, until the first fracture reveals the damage.
2.3 Bone Strength: More Than Just Bone Density
While bone mineral density (BMD) is a critical measurement, bone strength is influenced by several factors:
Bone geometry — size, shape, and thickness of bone.
Micro-architecture — the three-dimensional structure of trabecular (spongy) bone.
Turnover rate — the balance between bone formation and resorption.
Mineralization — proper deposition of calcium and phosphate in bone tissue.
Collagen quality — healthy collagen fibers add flexibility, helping bone resist fractures.
In other words, two people with the same BMD may have very different fracture risks, depending on these quality factors.
2.4 Primary vs. Secondary Osteoporosis
Osteoporosis can be classified into two broad categories:
Primary Osteoporosis
Postmenopausal (Type I): Related to the rapid bone loss after menopause due to estrogen deficiency.
Age-related (Senile, Type II): Occurs in both men and women as bone formation naturally slows with aging.
Secondary Osteoporosis
Caused by other diseases, medications, or conditions such as:Chronic glucocorticoid use (e.g., prednisone)
Rheumatoid arthritis
Chronic kidney disease
Hyperthyroidism or hyperparathyroidism
Malabsorption syndromes (e.g., celiac disease)
2.5 Fractures: The Defining Event
A person can have low bone mass without fractures — that’s called osteopenia, a “warning zone” before full osteoporosis. But once bone fragility leads to a low-trauma fracture (like from standing height or less), osteoporosis is essentially confirmed, even without a DXA scan.
The most common fracture sites are:
Vertebrae (spine)
Hip
Wrist (distal radius)
Humerus (upper arm)
2.6 How Osteoporosis Differs From Other Bone Diseases
Osteoporosis is sometimes confused with other skeletal disorders:
Osteomalacia — soft bones due to vitamin D deficiency, different mechanism.
Osteogenesis imperfecta — genetic “brittle bone” disease.
Paget’s disease — disorganized bone remodeling.
Osteoporosis is specifically about loss of bone mass and structure over time, most often due to aging and hormonal changes, though other causes exist.
2.7 A Visual Analogy
Imagine a well-built brick wall:
In youth, the bricks (minerals) are tightly packed, the mortar (collagen) is strong, and the wall is thick and stable.
Over time, tiny chips (microdamage) occur. If repairs slow down while damage continues, bricks fall out and gaps widen. Eventually, the wall looks intact from a distance but crumbles when pressed.
That’s osteoporosis in a nutshell — a structure that looks fine until it’s tested.
2.8 Why the Name Matters
Using the precise term osteoporosis matters in clinical settings because:
It signals high fracture risk to clinicians, prompting prevention and treatment.
It qualifies patients for certain medications or insurance coverage.
It helps differentiate from osteopenia (milder bone loss) or other bone diseases.
2.9 Key Takeaways
Osteoporosis = low bone quantity + poor bone quality.
It’s a silent disease until fractures occur.
Diagnosis is based on BMD (T-scores) and/or presence of fragility fractures.
It’s common, preventable, and treatable — but only if recognized early.
✅ This section sets a clear, thorough foundation so the rest of the guide can build on it.
3: Why “Premature Aging”? A Metaphor That Matters
When health professionals describe osteoporosis as “premature aging of the skeleton,” they aren’t just being poetic — they’re pointing to a biological truth that reframes the way we think about bone health.
The metaphor is powerful because it makes the invisible nature of osteoporosis easier to understand: your bones may be chronologically the age of your birth certificate, but if you have osteoporosis, their biological age may be years — even decades — older.
3.1 The Biology of Aging in Bone
Aging naturally affects all tissues, and bone is no exception. In healthy aging:
Bone mass peaks around the late 20s to early 30s — this is your “bone bank account.”
After peak bone mass, there is a slow decline in both bone density and micro-architectural integrity.
Hormonal shifts (especially estrogen and testosterone) accelerate this decline in midlife.
Over decades, osteoclast activity (bone breakdown) outpaces osteoblast activity (bone building).
In osteoporosis, these changes happen faster and to a greater degree than expected for one’s age — hence “premature aging.”
3.2 Why This Metaphor Matters for Awareness
Metaphors shape perception.
If osteoporosis is framed simply as “a disease for old people,” younger and middle-aged adults tune out — they assume it’s irrelevant until they’re 70.
But if it’s described as “premature aging of the skeleton,” the conversation shifts:
People realize bone health is a lifelong investment.
Risk factors in youth (poor diet, smoking, lack of exercise) are seen as accelerating “bone aging.”
Early screening feels logical, not optional.
3.3 What “Premature Aging” Looks Like Clinically
Imagine two women, both 55:
Jane has maintained strong habits: balanced diet, weight-bearing exercise, no smoking, and healthy hormones. Her bones might test like those of an average 50-year-old.
Sara has had early menopause at 42, a sedentary job, low calcium intake, and long-term steroid use for asthma. Her bone density scan might resemble that of a typical 70-year-old — a 15–20 year “aging leap”.
This “gap” between chronological and biological bone age explains why some people experience fractures decades earlier than peers.
3.4 Risk Factors That Accelerate Bone Aging
The skeleton can “age” prematurely due to:
Hormonal changes — early menopause, hypogonadism in men.
Chronic illness — inflammatory diseases, endocrine disorders.
Lifestyle factors — smoking, heavy alcohol use, low physical activity.
Nutritional deficits — chronic low calcium or vitamin D intake, eating disorders.
Medications — glucocorticoids, certain cancer treatments, antiepileptics.
Genetics — family history of fractures.
3.5 The Emotional Impact of the Metaphor
The idea of “premature aging” resonates because it taps into a universal fear: aging before your time.
It motivates people to:
Take preventive action earlier.
View osteoporosis not as inevitable but as something modifiable.
Understand that aging is not just about wrinkles and gray hair — it’s also about hidden tissue changes.
3.6 Limitations of the Metaphor
While useful, the metaphor has limits:
Not all osteoporosis is “premature” — age-related bone loss is normal.
Some causes are sudden (e.g., chemotherapy), not slow aging.
Overemphasis on “aging” could discourage older adults from seeking treatment (“it’s just my age”).
This is why clinicians must balance the metaphor with clear explanations of cause, prevention, and treatment.
3.7 Key Takeaways
Premature aging of the skeleton means bone health has declined faster than expected for your age.
The metaphor is effective for education and prevention messaging.
Lifestyle, hormones, disease, and medications can all accelerate skeletal aging.
Recognizing risk early can prevent decades of avoidable bone fragility.
✅ Now we’ve built the narrative bridge — readers will understand why osteoporosis isn’t just “an old person’s problem” and why early prevention is critical.
4: Bone Biology 101 — Remodeling, Hormones, and Micro-architecture
Understanding osteoporosis requires first understanding how healthy bone works. Bone is often mistaken for a static, lifeless material — like concrete — but in reality, it’s living, dynamic tissue that’s constantly being broken down and rebuilt.
This ongoing process, called bone remodeling, is essential for:
Maintaining bone strength
Repairing micro-damage from everyday activities
Regulating mineral balance in the body (especially calcium and phosphate)
When remodeling is balanced, skeletal integrity is preserved. In osteoporosis, bone breakdown outpaces bone building, leading to reduced mass and weaker structure.
4.1 Bone Structure: Two Main Types
Bone is organized into two major types of tissue:
Cortical (Compact) Bone
Dense, solid outer layer
Makes up ~80% of skeletal mass
Provides most of the structural strength
Found in shafts of long bones (femur, humerus) and outer shell of other bones
Trabecular (Spongy or Cancellous) Bone
Porous, honeycomb-like structure
Found in vertebrae, pelvis, ends of long bones
Metabolically more active — remodels faster
More vulnerable to rapid loss in osteoporosis
4.2 Bone Cells: The Remodeling Team
Three main cell types orchestrate bone health:
Osteoclasts — “Bone Demolition Crew”
Large, multinucleated cells that break down old or damaged bone (resorption). They dissolve the mineral part with acid and degrade the collagen framework with enzymes.Osteoblasts — “Construction Workers”
Cells that build new bone by producing collagen (type I) and controlling mineralization with calcium and phosphate.Osteocytes — “The Supervisors”
Former osteoblasts embedded within the bone matrix; they act as sensors, detecting mechanical stress and micro-damage, and signaling when remodeling is needed.
4.3 The Bone Remodeling Cycle
A single remodeling cycle takes about 3–6 months and happens in many microscopic spots across the skeleton at once. The cycle has five phases:
Activation — Osteocytes detect microdamage or a need for mineral release; they send chemical signals.
Resorption — Osteoclasts attach to bone and dissolve a small section.
Reversal — The surface is cleaned up, and osteoclasts undergo apoptosis (programmed death).
Formation — Osteoblasts lay down new collagen (osteoid), which is later mineralized.
Resting — The bone surface becomes inactive until the next cycle.
In osteoporosis, either:
Resorption is too high (excess osteoclast activity),
Formation is too low (insufficient osteoblast work), or
Both.
4.4 Hormonal Regulation of Bone
Hormones play a huge role in maintaining remodeling balance:
Estrogen
Inhibits bone resorption by reducing osteoclast lifespan and activity. Loss of estrogen (postmenopause) leads to a sharp rise in bone breakdown.Testosterone
Stimulates bone formation and is partly converted to estrogen in men, helping maintain bone mass.Parathyroid Hormone (PTH)
Regulates calcium levels; in small pulses, it can stimulate bone formation, but chronically high levels cause bone loss.Vitamin D
Enhances calcium absorption from the gut; low vitamin D means the body pulls more calcium from bone.Calcitonin
Mildly inhibits osteoclast activity (less significant in humans than other hormones).Cortisol (Glucocorticoids)
In excess, suppresses osteoblasts, increases resorption, and reduces calcium absorption — a major cause of secondary osteoporosis.
4.5 Micro-architecture: The Hidden Strength
Bone strength isn’t just about density — it’s also about the integrity of its internal scaffolding.
Trabecular Bone Micro-architecture:
In healthy bone, trabeculae (struts) are thick, interconnected, and evenly spaced.
In osteoporosis, trabeculae become thin, disconnected, and sometimes completely lost — like removing crossbeams from a bridge.Cortical Bone Porosity:
With age and disease, cortical bone develops microscopic holes, reducing stiffness and load-bearing ability.
Both changes drastically reduce fracture resistance, even if bone density hasn’t dropped dramatically.
4.6 Mechanical Stress and Bone Health
Bone follows Wolff’s Law: it adapts to the loads placed upon it.
Weight-bearing and resistance exercises stimulate osteocytes to signal more bone building.
Lack of mechanical stress (bed rest, space flight, sedentary lifestyle) triggers bone loss — often rapidly.
This is why astronauts lose significant bone mass in microgravity and why physical inactivity in older adults accelerates osteoporosis.
4.7 Key Takeaways
Bone is a living tissue in constant turnover.
Osteoporosis results when bone resorption outpaces bone formation.
Hormones, nutrition, and physical activity are critical regulators.
Micro-architecture is as important as density in determining fracture risk.
Protecting bone health is about preserving both quantity and quality.
✅ This section equips the reader with the biological framework to understand why osteoporosis happens and how treatments target specific parts of the remodeling process.
5: How Common Is Osteoporosis? (And Why It’s Underdiagnosed)
Osteoporosis is one of the most widespread chronic conditions in the world — yet it remains invisible in public awareness and surprisingly under-recognized in clinical practice. The irony is that it is both highly prevalent and highly preventable, but it often escapes detection until a fracture occurs.
5.1 Global Prevalence
The International Osteoporosis Foundation (IOF) estimates:
Over 200 million people worldwide are living with osteoporosis right now.
In many developed nations, 1 in 3 women and 1 in 5 men over 50 will experience an osteoporotic fracture in their lifetime.
Regional snapshots:
United States
~10 million have osteoporosis.
Another 43 million have low bone mass (osteopenia), putting them at high risk.
Europe
~27.5 million people have osteoporosis.
3.5 million new fragility fractures occur every year.
Asia-Pacific
The aging population in China, Japan, and Southeast Asia is expected to triple osteoporosis cases by 2050.
Middle East & Africa
Data is less comprehensive, but rising life expectancy and urban lifestyles are increasing risk.
5.2 Age and Gender Trends
Women are at higher risk due to:
Lower peak bone mass than men.
Sharp estrogen drop after menopause.
Men tend to develop osteoporosis later, but when they do:
Fractures are often more serious.
Mortality after hip fracture is higher in men than women.
Younger people are not immune:
Secondary osteoporosis (due to illness, medications, or lifestyle) is increasingly diagnosed in individuals under 50.
5.3 The Burden of Fragility Fractures
Fractures are the most telling indicator of osteoporosis prevalence:
In the U.S., over 2 million osteoporotic fractures occur each year.
Hip fractures are the most feared:
20–30% mortality within the first year.
Up to 50% of survivors lose the ability to live independently.
Vertebral fractures are underreported:
Many are silent and only found incidentally on X-rays.
They cause progressive height loss, kyphosis (stooped posture), and chronic pain.
5.4 Why So Many Cases Go Undiagnosed
Osteoporosis is underdiagnosed for several reasons:
Silent Progression
No pain or symptoms until a fracture occurs.
Many people believe bone loss is a normal, unavoidable part of aging.
Screening Gaps
Many at-risk individuals have never had a DXA scan.
Guidelines recommend screening women ≥65 and men ≥70, but compliance is low.
Younger adults with secondary risk factors are often overlooked.
Healthcare Priorities
Physicians may focus on treating acute conditions (e.g., fractures, arthritis pain) rather than proactive bone health.
Post-Fracture Neglect
Up to 80% of fracture patients never receive an osteoporosis evaluation or treatment afterward — a missed opportunity to prevent the next fracture.
Public Misunderstanding
People often confuse osteoporosis with osteoarthritis, assuming it’s about joint pain rather than bone fragility.
5.5 Hidden Cases in “Osteopenia”
Osteopenia — the stage before osteoporosis — affects a much larger group than osteoporosis itself.
Many osteopenic patients already have a fracture risk high enough to warrant treatment.
This is especially true in elderly individuals, where falls are more frequent and bone strength is already compromised by micro-architectural changes.
5.6 The Future: A Growing Epidemic
Population Aging: By 2050, the proportion of people over 65 will double globally.
Urban Lifestyle Changes: Less outdoor activity, lower sun exposure (vitamin D), and more sedentary habits are fueling bone loss earlier in life.
Survivorship of Chronic Illness: Advances in medicine mean more people live long enough for osteoporosis to develop — or to suffer secondary bone loss from treatments.
5.7 Key Takeaways
Osteoporosis is extremely common and affects hundreds of millions globally.
Women are more likely to develop it, but men have higher post-fracture mortality.
Screening and post-fracture treatment rates are far below optimal.
Without changes in awareness, prevention, and diagnosis, fracture numbers will skyrocket in the coming decades.
✅ This section makes it clear that osteoporosis isn’t rare at all — it’s under-recognized.
6: Risk Factors — The Usual Suspects and the Sneaky Ones
Osteoporosis doesn’t develop overnight. It’s the result of multiple influences that affect bone mass, quality, and turnover over years or decades. Some factors are unavoidable, like age and genetics. Others are modifiable, meaning you can take steps to reduce their impact.
To make this practical, we’ll divide them into two categories:
The Usual Suspects — well-known, common drivers.
The Sneaky Ones — lesser-known or overlooked contributors.
6.1 The Usual Suspects
These are the most recognized risk factors, widely accepted in medical guidelines.
1. Age
Why it matters: Bone mass peaks in the late 20s–early 30s, then slowly declines. Aging also reduces osteoblast activity (bone building) and increases micro-architectural deterioration.
Impact: Older adults are at higher fracture risk even if bone density is only moderately reduced.
2. Female Sex
Women have:
Lower peak bone mass compared to men.
Sharp bone loss after menopause due to estrogen drop.
Menopause-related loss can be up to 20% of bone mass in the first 5–7 years.
3. Postmenopausal Status
Mechanism: Estrogen protects bone by inhibiting osteoclast activity. Loss of estrogen speeds up bone resorption.
Special note: Early menopause (<45 years) or surgical removal of ovaries increases lifetime risk.
4. Family History
If a parent had a hip fracture, your risk is significantly higher — partly due to inherited bone structure, partly due to shared lifestyle factors.
5. Low Body Weight / BMI
BMI <19 is linked to lower bone mass.
Less fat tissue means less estrogen production after menopause.
6. Previous Fracture
A low-trauma fracture after age 50 is one of the strongest predictors of future fractures.
6.2 The Sneaky Ones
These factors often fly under the radar — many people (and even some healthcare providers) don’t think of them as bone-related.
1. Certain Medications
Glucocorticoids (steroids) — e.g., prednisone, used for asthma, autoimmune disorders. Even low doses over long periods increase fracture risk.
Aromatase inhibitors — for breast cancer treatment, drastically reduce estrogen.
Androgen deprivation therapy — for prostate cancer, lowers testosterone.
Some anticonvulsants — affect vitamin D metabolism (phenytoin, phenobarbital).
SSRIs (antidepressants) — associated with increased fracture risk, possibly due to serotonin’s role in bone metabolism.
Proton pump inhibitors (PPIs) — long-term use can reduce calcium absorption.
2. Chronic Illnesses
Endocrine disorders: Hyperthyroidism, hyperparathyroidism, diabetes.
Inflammatory diseases: Rheumatoid arthritis, inflammatory bowel disease.
Chronic kidney disease: Alters calcium, phosphate, and vitamin D regulation.
Celiac disease: Malabsorption of calcium and vitamin D.
3. Lifestyle Factors
Smoking: Nicotine and other toxins directly damage bone cells and reduce estrogen levels.
Alcohol: Heavy drinking interferes with calcium absorption and increases fall risk.
Sedentary lifestyle: Without regular mechanical loading, bones weaken.
Low calcium/vitamin D intake: Weakens bone formation from childhood onward.
4. Nutritional Red Flags
Chronic dieting or eating disorders.
Very high caffeine or salt intake — both can increase calcium loss in urine.
Diets chronically low in protein — impairs collagen production in bone.
5. Falls and Poor Balance
Weak muscles, vision problems, or poor coordination don’t cause osteoporosis directly, but they dramatically increase the chance of fractures in someone with fragile bones.
6. Hormonal Changes in Men
Hypogonadism (low testosterone) can occur from aging, pituitary disease, or medical treatment. Testosterone loss contributes to both bone and muscle decline.
6.3 The “Risk Factor Stack”
Osteoporosis risk isn’t just about one factor — it’s about the cumulative load:
A postmenopausal woman with low BMI and a smoking habit has a much higher risk than a peer with only one of those factors.
Risk factors often interact — e.g., a sedentary lifestyle + chronic illness + steroid use can accelerate bone loss dramatically.
6.4 Red Flags That Should Trigger Screening
Any adult fracture after age 50.
Early menopause or loss of menstrual periods for >6 months (not pregnancy-related).
Long-term steroid therapy (>3 months).
Unexplained height loss (>4 cm / ~1.5 inches).
Chronic digestive disorders affecting nutrient absorption.
6.5 Key Takeaways
Many osteoporosis risks are hidden in plain sight — you may have them without realizing their impact on your skeleton.
The more risk factors you have, the earlier you should start screening and prevention.
Addressing modifiable risks (diet, exercise, smoking, alcohol, medication review) can significantly slow or even prevent osteoporosis.
✅ Now the reader knows exactly what can put them on the path to osteoporosis — from the obvious to the unexpected.
7: Signs and Symptoms — The Silent Thief
Osteoporosis is often called the “silent thief” because it quietly steals bone density over the years without causing pain or obvious symptoms. Most people don’t even know they have it until a fracture occurs.
But while early signs are subtle, there are clues — if you know what to look for.
7.1 Why It’s Often Symptomless
Bone has no pain receptors. Losing density doesn’t hurt — until the structure becomes so weak that tiny cracks (microfractures) or full fractures occur.
The first “symptom” is often a fracture from a low-impact event, such as:
Falling from standing height.
Lifting a heavy object and feeling sudden back pain.
Even coughing or sneezing in severe cases.
7.2 Early & Subtle Signs
These often appear before the first fracture:
Loss of Height
Gradual shrinking — sometimes unnoticed until clothes fit differently or friends comment.
Caused by compression fractures in the spine.
Loss of >4 cm (1.5 inches) is a red flag.
Stooped Posture (Kyphosis)
Rounded upper back, sometimes called a “dowager’s hump.”
Results from vertebrae collapsing and changing spinal alignment.
Back Pain Without Injury
Persistent, dull, or sharp pain in the mid-to-lower back.
Can be due to small vertebral fractures.
Weak Grip Strength
Linked in studies to low bone mineral density and higher fall risk.
May reflect general muscle loss that accompanies bone loss.
Nail & Hair Changes
More brittle nails or hair thinning aren’t specific to osteoporosis, but can accompany nutritional deficiencies affecting bone.
7.3 Symptoms of Moderate to Severe Osteoporosis
These are usually signs that the disease has been present for years:
Frequent Fractures
Wrist, hip, spine are most common.
Hip fractures can be life-changing — many require surgery and long rehab.
Sudden Severe Back Pain
From an acute compression fracture.
Pain may worsen with standing or walking, and improve when lying down.
Spinal Deformity
Progressive stooping, abdomen protrusion, rib cage resting closer to the pelvis.
Loss of Mobility
From both bone fragility and the fear of falling.
7.4 How It’s Often Discovered
Osteoporosis is frequently diagnosed after:
An X-ray for another reason shows thinner bones or fractures.
A bone density scan (DEXA) is done due to risk factors.
A fracture happens after minimal trauma.
7.5 The Psychological Impact of Symptoms
It’s not just the physical changes:
Fear of movement after a fracture can cause people to avoid activity — which worsens bone loss.
Height loss and posture changes can affect self-esteem and social interaction.
Chronic pain can lead to depression and reduced quality of life.
7.6 Key Takeaways
Osteoporosis may be invisible for years — but it leaves subtle footprints in posture, height, and strength.
The earlier these signs are recognized, the sooner prevention or treatment can start.
Never ignore unexplained height loss, chronic back pain, or fractures from minor incidents — they’re your skeleton’s way of saying, “Check me out!”
✅ With this section, the reader understands why osteoporosis is dangerous even before the first fracture and what to watch for in themselves or loved ones.
8: How Doctors Diagnose It (DXA, T-scores, and More)
Osteoporosis can’t be diagnosed by guessing from symptoms — because in most cases, there aren’t any early symptoms at all.
The only way to know for sure is through objective measurement of bone strength, combined with an assessment of your risk factors and history.
8.1 The Two Main Goals of Diagnosis
Identify low bone density before fractures occur — prevention is always better than recovery.
Find and address secondary causes — like vitamin D deficiency, thyroid problems, or medications that harm bone.
8.2 The DXA (Dual-energy X-ray Absorptiometry) Scan
The gold standard for measuring bone mineral density (BMD).
How it works:
Uses low-dose X-rays at two energy levels to measure bone density.
Usually targets:
Lumbar spine (L1–L4)
Hip (total hip & femoral neck)
Sometimes forearm (if spine/hip can’t be measured).
Advantages:
Quick (5–10 minutes)
Painless
Very low radiation (less than a chest X-ray)
8.3 Understanding T-Scores and Z-Scores
DXA results come with two numbers:
T-score — compares your bone density to a healthy young adult of the same sex.
Normal: T-score ≥ -1.0
Osteopenia (low bone mass): -1.0 to -2.5
Osteoporosis: ≤ -2.5
Severe osteoporosis: ≤ -2.5 plus a fragility fracture
Z-score — compares your bone density to someone your age, sex, and size.
Z-score < -2.0 suggests bone loss is from something other than normal aging (secondary osteoporosis).
8.4 Other Imaging Methods
While DXA is the standard, other tools may be used:
Quantitative Computed Tomography (QCT):
3D imaging, can measure trabecular bone quality.
More radiation, higher cost.
Trabecular Bone Score (TBS):
An add-on to DXA that estimates bone microarchitecture quality.
Vertebral Fracture Assessment (VFA):
Performed with DXA to detect silent spine fractures.
8.5 Laboratory Tests
To check for causes or contributors to bone loss:
Calcium (blood and urine)
Vitamin D (25-hydroxyvitamin D)
Parathyroid hormone (PTH)
Thyroid-stimulating hormone (TSH)
Liver and kidney function tests
Sex hormones (estrogen, testosterone)
Markers of bone turnover (e.g., CTX, P1NP)
8.6 Fracture Risk Assessment Tool (FRAX)
Even with DXA, fracture risk can vary between individuals with the same bone density.
FRAX calculates your 10-year probability of:
Major osteoporotic fracture (hip, spine, forearm, shoulder)
Hip fracture specifically
It combines:
Age, sex, weight, height
Previous fractures
Parental hip fracture
Smoking, alcohol intake
Glucocorticoid use
Rheumatoid arthritis
DXA results (optional but preferred)
Why FRAX matters:
Two people with the same T-score may have different treatment needs if their overall fracture risk differs.
8.7 When to Get Tested
Guidelines vary, but common recommendations are:
Women ≥65 years old
Men ≥70 years old
Adults ≥50 years with:
A fragility fracture
Major risk factors (e.g., steroids, early menopause, low body weight)
Postmenopausal women with risk factors, even before 65
8.8 Pitfalls in Diagnosis
False reassurance: Normal DXA doesn’t mean no risk — fractures can still happen in osteopenia if risk factors are high.
Measurement variability: Different machines, or even the same machine over time, can give slightly different results — consistency matters.
Underuse of spine imaging: Silent vertebral fractures are often missed unless specifically checked.
8.9 Key Takeaways
DXA scan + clinical assessment = best diagnosis.
T-scores tell you where you stand; FRAX tells you where you might be headed.
Finding osteoporosis early gives you a much bigger chance to prevent devastating fractures.
9: Fracture Risk — FRAX and Clinical Judgment
Bone density is only one piece of the puzzle when it comes to predicting fractures.
A person with “mild” bone loss (osteopenia) can sometimes have a higher fracture risk than someone with osteoporosis — depending on age, history, and other factors.
That’s why modern osteoporosis care combines numbers from a DXA scan with real-life risk factors to get the full picture.
9.1 Why Fracture Risk Matters
Fractures are the true danger of osteoporosis.
Bone loss itself doesn’t hurt — it’s the broken bones (especially hip and spine) that cause pain, disability, and reduced life expectancy.Knowing fracture risk helps decide:
Who needs treatment now
Who can focus on lifestyle changes and monitoring
9.2 The FRAX Tool in Detail
FRAX = Fracture Risk Assessment Tool
Developed by the University of Sheffield, used worldwide, with region-specific adjustments.
Inputs:
Age, sex, weight, height
Prior fracture history
Parental hip fracture history
Current smoking
Glucocorticoid use (e.g., prednisone)
Rheumatoid arthritis
Secondary osteoporosis causes (e.g., type 1 diabetes, untreated hyperthyroidism)
Alcohol (≥3 units/day)
Bone Mineral Density (optional, but improves accuracy)
Outputs:
10-year risk of major osteoporotic fracture (hip, spine, shoulder, or forearm)
10-year risk of hip fracture alone
9.3 Interpreting FRAX Scores
Guidelines differ by country, but common thresholds for considering medication are:
Major osteoporotic fracture risk ≥20%
Hip fracture risk ≥3%
Example:
68-year-old woman, T-score -2.0 (osteopenia), plus smoking and parental hip fracture →
FRAX may show hip fracture risk above 3% → Treatment may be recommended even without osteoporosis-level T-score.
9.4 Limitations of FRAX
Doesn’t count falls — a big risk factor in elderly patients.
May underestimate risk in people with multiple recent fractures.
Not ideal for younger patients (<40 years old).
Assumes “average” doses for steroids — may not fit very high or low doses.
9.5 Clinical Judgment: Beyond FRAX
Doctors don’t use FRAX alone. They also look at:
Number and severity of previous fractures
Recent fractures (within last 2 years = higher risk)
Bone turnover markers
Fall history and balance problems
Medications (e.g., aromatase inhibitors in breast cancer)
Comorbidities (e.g., chronic kidney disease)
9.6 Risk Categories in Practice
Doctors often place patients into three categories:
Low risk
T-score ≥ -1.0
FRAX scores below thresholds
No major risk factors
→ Lifestyle changes + calcium/vitamin D, no medication.
Moderate risk
Osteopenia on DXA
FRAX at or near treatment threshold
→ Consider meds if other risk factors present.
High risk
Osteoporosis on DXA
High FRAX score or previous fragility fracture
→ Medication strongly recommended.
Very high risk
Multiple fractures, very low T-score (e.g., -3.5), or recent hip/spine fracture
→ Aggressive treatment (possibly anabolic drugs first).
9.7 The Role of Patient Preference
Some people:
Prefer early medication to reduce fracture anxiety.
Prefer to delay meds and try lifestyle changes first — but with close monitoring.
Shared decision-making ensures the plan fits medical evidence + patient values.
9.8 Key Takeaways
Bone density + risk factors = real fracture risk.
FRAX helps guide treatment decisions, but it’s not a substitute for a doctor’s judgment.
The higher the risk, the more urgent the need for intervention — especially to prevent a first or second fracture.
10: Complications — Why Fractures Change Everything
Osteoporosis is often described as a silent disease — but when complications appear, they can be loud, life-changing, and permanent.
The first fracture is often the turning point in a patient’s health journey, sometimes referred to as a “sentinel event” because it signals both current bone fragility and high risk of future fractures.
10.1 Why Fractures Matter More Than Low Bone Density
Low bone density is an invisible number on a scan.
A fracture, on the other hand, is:
Painful
Functionally limiting
Often a trigger for rapid physical decline
Many patients recover incompletely — and some never return to their pre-fracture level of independence.
10.2 The Three Big Fracture Sites
While osteoporosis can weaken bones anywhere, three locations cause the greatest long-term harm:
Hip fractures
Usually caused by a fall from standing height.
Often require surgery (hip replacement or fixation).
Associated with:
High mortality: up to 20–30% within one year in older adults.
Loss of independence: 50% need long-term care after.
Chronic pain and reduced mobility.
Vertebral (spinal) fractures
Can happen spontaneously or from minor movements (e.g., bending over).
Symptoms:
Sudden severe back pain (acute fracture)
Gradual height loss, stooped posture (kyphosis)
Compression of lungs → breathing difficulty
Compression of abdomen → digestive problems
Often undetected — only 1/3 are diagnosed.
Wrist fractures (Colles’ fracture)
Often first visible sign of osteoporosis.
Although less deadly than hip fractures, they:
Limit hand function.
Reduce independence in daily tasks.
Predict higher risk of later hip or spine fractures.
10.3 Secondary Complications After a Fracture
Fractures trigger a cascade of other health problems:
Muscle deconditioning: weeks to months of reduced movement → loss of muscle mass and balance.
Blood clots (DVT/PE): risk rises with immobility.
Pneumonia: from prolonged bed rest or reduced lung capacity after spinal fractures.
Depression & anxiety: fear of falling can cause social withdrawal.
Chronic pain: can persist long after bone healing.
10.4 The “Fracture Cycle”
One fracture increases the likelihood of another — often within the next 12–24 months.
Reasons:
Weakened bone architecture (microdamage).
Reduced mobility → weaker muscles → more falls.
Underlying risk factors not yet treated.
10.5 Economic & Social Impact
Fractures aren’t just a personal health issue — they are a public health burden:
Healthcare costs: hip fracture treatment can exceed $40,000 USD in the first year.
Work loss: in younger patients, recovery time can mean lost income.
Family impact: caregiving demands increase stress and financial strain.
10.6 Preventing the First and Second Fracture
Bone-strengthening medication when indicated.
Fall prevention strategies: home safety checks, balance training, vision correction.
Rehabilitation: after a fracture, early mobilization and targeted physical therapy reduce complications.
10.7 Key Takeaways
Osteoporosis complications aren’t just medical — they affect independence, mood, social life, and survival.
Preventing fractures is the core mission of osteoporosis treatment.
Once a fracture happens, fast intervention is crucial to break the cycle.
11: Treatment Strategy — Think in Phases and “Sequence”
Osteoporosis treatment is most effective when it’s strategic, not random.
Rather than throwing all options at a patient at once, clinicians aim to sequence therapy — delivering the right intervention at the right stage, for the right patient.
11.1 Why “Phases” Matter
Bone is a living, dynamic tissue.
Some treatments build new bone, others slow bone loss.
If we use them in the wrong order, we can blunt their effectiveness.
Example:
Starting a potent antiresorptive (like a bisphosphonate) before an anabolic (like teriparatide) may reduce the anabolic’s bone-building benefit.
This is why sequencing matters.
11.2 The Three Core Phases of Osteoporosis Management
Phase 1: Risk Identification & Immediate Protection
Goal: Prevent the first fracture (or the next one if already fractured).
Assess fracture risk: DXA scan, FRAX score, and clinical history.
Address reversible risks:
Correct vitamin D and calcium deficiency.
Review medications that may weaken bone (e.g., glucocorticoids).
Initiate urgent therapy for very high-risk patients:
Recent fracture within the last 2 years.
Multiple vertebral fractures.
Very low T-score (< -3.0).
Phase 2: Targeted Pharmacologic Therapy
Goal: Actively improve bone strength.
Two main categories of drugs — often sequenced:
Anabolic agents (bone builders)
Examples: Teriparatide, Abaloparatide, Romosozumab.
Mechanism: Stimulate osteoblasts → form new bone matrix.
Duration: Usually limited to 12–24 months.
Best for: Very high fracture risk, multiple fractures, severe bone loss.
Antiresorptive agents (bone loss stoppers)
Examples: Bisphosphonates (Alendronate, Zoledronic acid), Denosumab.
Mechanism: Reduce osteoclast activity → slow bone breakdown.
Best for: Long-term maintenance after anabolic therapy or moderate fracture risk.
Key sequencing principle:
Start with anabolic → then switch to antiresorptive for long-term benefit.
If starting directly with antiresorptive, know that later switching to anabolic will give smaller gains.
Phase 3: Maintenance & Monitoring
Goal: Preserve gains and prevent relapse.
Transition to maintenance therapy:
Most patients stay on antiresorptives long-term.
Some may take “drug holidays” (temporary breaks) from bisphosphonates after 3–5 years if risk is low.
Regular follow-up:
DXA every 1–2 years.
Monitor calcium, vitamin D, kidney function.
Lifestyle reinforcement:
Weight-bearing and resistance exercise.
Balance training to prevent falls.
Adequate nutrition.
11.3 The “Very High-Risk” Treatment Pathway
Patients with:
Hip or vertebral fracture in the past year.
Multiple fragility fractures.
Extremely low bone density (T-score ≤ -3.5).
Recommended sequence:
Start with an anabolic agent for 12–18 months.
Immediately follow with potent antiresorptive (Zoledronic acid or Denosumab) to “lock in” gains.
Continue lifestyle + supplementation indefinitely.
11.4 Special Considerations
Renal impairment: Avoid some bisphosphonates; denosumab may be preferred.
Glucocorticoid-induced osteoporosis: Early intervention is critical, often with anabolic-first strategy.
Younger postmenopausal women: Weigh benefits vs. long-term medication exposure.
11.5 Why Stopping Treatment Abruptly Can Be Dangerous
Certain drugs (especially Denosumab) cause rapid bone loss and rebound fractures if stopped suddenly without another medication to follow.
This is why planned sequencing is essential, not optional.
11.6 Summary Table: Strategic Sequencing
Step
Primary Goal
Typical Treatment
Phase 1
Rapid fracture risk reduction
Supplements, fall prevention, urgent medication
Phase 2
Build or preserve bone
Anabolic (build) → Antiresorptive (maintain)
Phase 3
Maintain gains & prevent relapse
Long-term antiresorptive, lifestyle, monitoring
Bottom line:
Osteoporosis treatment works best when it’s personalized, phased, and carefully sequenced — not rushed and not random.
12: Medications — What Works, How It Works, and Key Caveats
Osteoporosis medication choices depend on fracture risk, bone density, patient profile, and treatment sequence strategy.
All drugs aim to shift the bone remodeling balance in favor of bone gain or reduced loss — but they achieve this through different biological pathways.
12.1 The Two Big Categories
Antiresorptives — Slow down bone breakdown by inhibiting osteoclasts.
Anabolics — Build new bone by stimulating osteoblasts.
A third category (mixed action) includes drugs like Romosozumab, which do both.
12.2 Antiresorptive Medications
These drugs target osteoclast-mediated bone resorption.
They don’t usually create new bone, but they preserve what’s there — and over time, bone density can increase.
12.2.1 Bisphosphonates
Examples: Alendronate, Risedronate, Ibandronate, Zoledronic acid.
Mechanism: Attach to bone mineral; when osteoclasts try to resorb bone, they ingest the drug and undergo apoptosis (cell death).
Administration:
Oral: weekly or monthly (Alendronate, Risedronate, Ibandronate).
IV: yearly (Zoledronic acid), quarterly (Ibandronate).
Benefits:
Reduce vertebral, non-vertebral, and hip fractures (Zoledronic acid and Alendronate strongest evidence for hip).
Long track record, inexpensive generics available.
Side Effects:
Oral: esophagitis, GI upset (must remain upright after taking).
IV: flu-like symptoms after first dose.
Rare: osteonecrosis of the jaw (ONJ), atypical femur fractures.
Special Notes:
Good choice for maintenance phase after anabolic therapy.
Can consider “drug holiday” after 3–5 years if risk is low.
12.2.2 Denosumab
Brand name: Prolia.
Mechanism: Monoclonal antibody targeting RANKL (a signal required for osteoclast formation and function).
Administration: Subcutaneous injection every 6 months.
Benefits:
Potent fracture risk reduction (vertebral, non-vertebral, hip).
Works even in reduced kidney function.
Side Effects:
Hypocalcemia (especially if vitamin D deficient).
Skin infections (rare).
ONJ, atypical femur fractures (rare).
Key Caveat:
Stopping Denosumab abruptly causes rapid bone loss and multiple vertebral fractures — must transition immediately to another antiresorptive when stopping.
12.2.3 SERMs (Selective Estrogen Receptor Modulators)
Examples: Raloxifene, Bazedoxifene.
Mechanism: Mimic estrogen’s bone-protective effects in bone tissue, block estrogen effects in breast/uterus.
Administration: Daily oral tablet.
Benefits:
Reduces vertebral fractures.
May reduce breast cancer risk.
Side Effects:
Increases risk of deep vein thrombosis (DVT), hot flashes.
Best for:
Postmenopausal women with mild bone loss who also want breast cancer risk reduction.
12.2.4 Hormone Therapy
Estrogen ± progestin: Prevents bone loss; effective early after menopause.
Limitations: Not first-line solely for osteoporosis due to increased risks (breast cancer, stroke, heart disease).
Best for: Women within 10 years of menopause who also need menopausal symptom relief.
12.3 Anabolic Medications
These stimulate osteoblast activity — actively building new bone structure.
They are especially valuable for patients at very high fracture risk or with multiple recent fractures.
12.3.1 Teriparatide
Brand name: Forteo.
Mechanism: Synthetic parathyroid hormone fragment (PTH 1-34) given in daily pulses stimulates bone formation.
Administration: Daily self-injection.
Duration: Maximum 2 years in lifetime.
Benefits:
Large increases in spinal bone density; reduces vertebral and non-vertebral fractures.Side Effects: Hypercalcemia, leg cramps, dizziness.
Special Note: After stopping, must follow with antiresorptive to preserve gains.
12.3.2 Abaloparatide
Brand name: Tymlos.
Mechanism: PTHrP analog with similar bone-building action as Teriparatide.
Administration: Daily self-injection.
Duration: Maximum 2 years.
Benefits: Significant fracture risk reduction.
Side Effects: Similar to Teriparatide.
12.4 Mixed Action: Romosozumab
Brand name: Evenity.
Mechanism: Monoclonal antibody blocking sclerostin → increases bone formation and decreases resorption.
Administration: Monthly injections for 12 months.
Benefits:
Rapid bone density gains.
Reduces vertebral and clinical fractures.
Side Effects: Injection site reactions, possible cardiovascular risk (avoid in patients with recent heart attack/stroke).
Sequence Tip: Use for 1 year, then transition to antiresorptive.
12.5 Supplementation as a Medication Adjunct
Calcium: Usually 1000–1200 mg/day (diet + supplement).
Vitamin D: 800–2000 IU/day, individualized.
Not a replacement for prescription drugs in moderate-to-severe osteoporosis, but essential for all patients.
12.6 Choosing the Right Medication
Scenario
Preferred First Step
Very high risk with recent fracture
Anabolic first → Antiresorptive
High risk, no recent fracture
Antiresorptive first
Renal impairment
Denosumab or anabolic
Estrogen deficiency + menopause symptoms
Hormone therapy (if low CV risk)
Breast cancer risk reduction desired
SERM
Bottom line:
The osteoporosis medication landscape is diverse, but no single drug is best for everyone. The art is in matching the drug to the patient and sequencing it properly to get the maximum benefit with minimal risk.
13: Special Populations — Men, Pre-/Perimenopause, Glucocorticoids, CKD
Osteoporosis is often thought of as a postmenopausal women’s disease, but that’s an incomplete — and potentially dangerous — assumption.
Certain special populations face unique risk profiles, diagnostic challenges, and treatment considerations.
Failing to recognize osteoporosis in these groups can lead to late diagnosis and preventable fractures.
13.1 Men and Osteoporosis
Prevalence & Underdiagnosis
About 1 in 5 men over age 50 will experience an osteoporosis-related fracture.
Men are less likely to be screened, even after a fracture.
When men fracture, outcomes tend to be worse than in women — higher mortality and slower recovery.
Risk Factors in Men
Low testosterone (hypogonadism).
Long-term glucocorticoid use.
Excess alcohol use, smoking.
Chronic illnesses (e.g., COPD, rheumatoid arthritis).
Medications: androgen deprivation therapy for prostate cancer.
Diagnosis in Men
Same tools as women (DXA, T-score), but clinicians may also check:
Serum testosterone and other hormones.
Secondary causes like vitamin D deficiency, celiac disease, or chronic kidney disease.
Treatment Notes
Bisphosphonates, denosumab, and teriparatide are effective in men.
Address hormonal causes when possible.
Men benefit from resistance training and protein optimization.
13.2 Pre- and Perimenopausal Women
Why It’s Different
Bone loss in younger women may be secondary to another condition (not just hormonal changes).
Causes include:
Eating disorders.
Excessive exercise without adequate nutrition.
Amenorrhea (loss of menstruation).
Endocrine disorders (thyroid, parathyroid, adrenal).
Medications (glucocorticoids, anticonvulsants).
Diagnosis Caveats
T-scores aren’t always used in premenopausal women; Z-scores (age-matched) are preferred.
A Z-score ≤ -2.0 suggests bone loss not typical for age.
Treatment Priorities
Identify and treat underlying cause.
Medications are generally reserved for women with:
Recurrent fractures.
Ongoing high risk after addressing secondary causes.
Lifestyle and nutritional optimization are first-line.
13.3 Glucocorticoid-Induced Osteoporosis (GIOP)
Why It’s a Big Deal
Glucocorticoids (e.g., prednisone) accelerate bone loss rapidly — sometimes within the first 3–6 months.
They:
Reduce bone formation.
Increase bone resorption.
Decrease calcium absorption.
Who’s at Risk
Patients on ≥5 mg prednisone (or equivalent) daily for ≥3 months.
Common in asthma, autoimmune diseases, and post-transplant care.
Prevention & Management
Start preventive measures immediately — don’t wait for bone loss to appear.
Calcium, vitamin D, weight-bearing exercise.
Early initiation of bisphosphonates or other agents in high-risk patients.
13.4 Chronic Kidney Disease (CKD)
The CKD–Bone Connection
CKD alters mineral metabolism: imbalanced calcium, phosphate, and parathyroid hormone levels.
Leads to renal osteodystrophy, which may include osteoporosis-like changes.
Challenges in Diagnosis
DXA scans measure bone density but not bone quality — which may be abnormal in CKD.
Labs like PTH, alkaline phosphatase, and vitamin D help clarify the picture.
Treatment Cautions
Some osteoporosis drugs require caution or dose adjustments in CKD.
In advanced CKD, management often focuses on correcting mineral imbalances first.
13.5 Shared Principles Across Special Populations
Early recognition is key — these groups are often missed until a fracture occurs.
Secondary cause workup is essential.
Individualized treatment plans improve safety and outcomes.
Multidisciplinary care (endocrinology, nephrology, rheumatology, nutrition) often yields the best results.
✅ Key Takeaway:
Osteoporosis is not one-size-fits-all — men, younger women, people on steroids, and those with CKD require tailored diagnostic and treatment strategies. Early detection and proactive management can prevent life-altering fractures in these under-recognized groups.
14: Secondary Causes — Don’t Miss These
Not all osteoporosis is primary (age-related or postmenopausal).
A substantial proportion of cases — especially in men, younger women, and atypical presentations — are due to secondary causes.
These are underlying conditions, nutritional deficiencies, or medications that accelerate bone loss or weaken bone structure.
Recognizing and treating secondary causes can reverse bone loss or at least slow progression significantly.
14.1 Why This Matters
Mislabeling a patient as having “primary osteoporosis” when they actually have a secondary cause means:
You treat the symptom (bone loss) but not the root problem.
The patient’s fracture risk remains unnecessarily high.
Many secondary causes are treatable or modifiable.
14.2 Common Secondary Causes of Osteoporosis
A. Endocrine Disorders
Hyperthyroidism (overactive thyroid)
Increases bone turnover → bone resorption outpaces formation.
Can be from overt disease or excess thyroid hormone medication.
Hyperparathyroidism
Elevated parathyroid hormone draws calcium out of bones.
May be primary (tumor) or secondary (often due to vitamin D deficiency or CKD).
Cushing’s syndrome
Excess cortisol, whether from the adrenal glands or long-term steroid use.
Hypogonadism (low sex hormones)
Men: Low testosterone.
Women: Early menopause or ovarian failure.
B. Gastrointestinal Disorders
Celiac disease
Gluten-triggered autoimmune reaction damages the gut, reducing calcium and vitamin D absorption.
Inflammatory bowel disease (Crohn’s, ulcerative colitis)
Chronic inflammation + steroid treatment = high bone loss risk.
Bariatric surgery
Especially gastric bypass — limits nutrient absorption long term.
Chronic liver disease
Impaired vitamin D metabolism and protein synthesis.
C. Hematologic Disorders
Multiple myeloma
Malignant plasma cells directly damage bone.
Leukemia and lymphoma
Can increase bone breakdown and interfere with normal formation.
D. Chronic Kidney Disease (CKD)
Already covered in detail in Section 13.4, but here it’s worth noting:
CKD-MBD (mineral and bone disorder) is a frequent secondary cause.
E. Medications
Glucocorticoids
Discussed in Section 13.3 — rapid bone loss even at moderate doses.
Aromatase inhibitors
Used in breast cancer — dramatically reduce estrogen.
Androgen deprivation therapy
Used in prostate cancer — reduces testosterone.
Anticonvulsants (phenytoin, phenobarbital, carbamazepine)
Increase vitamin D breakdown.
Proton pump inhibitors (omeprazole, etc.)
Long-term use may reduce calcium absorption.
F. Nutritional Factors
Vitamin D deficiency
Common, often silent, but critical for calcium absorption.
Calcium deficiency
Low dietary intake or poor absorption.
Protein–energy malnutrition
Impairs collagen matrix production in bone.
G. Lifestyle & Environmental
Chronic alcohol overuse.
Heavy smoking.
Prolonged immobility (bed rest, paralysis).
14.3 How to Detect Secondary Osteoporosis
When a patient presents with osteoporosis earlier than expected or with an unusual fracture pattern, a workup is essential.
Typical laboratory evaluation may include:
Calcium, phosphate.
25-hydroxyvitamin D.
Parathyroid hormone (PTH).
Thyroid-stimulating hormone (TSH).
Testosterone (men) / estradiol (women).
Complete blood count.
Liver and kidney function tests.
Celiac antibodies.
Serum protein electrophoresis (if myeloma suspected).
14.4 Treating the Root Cause
Primary principle: Fix the underlying disorder when possible.
Examples:
Hyperthyroidism → restore normal thyroid levels.
Celiac disease → strict gluten-free diet.
Hypogonadism → hormone replacement (if safe and indicated).
Medication-induced → switch to alternatives or mitigate effects.
After addressing the root cause:
Continue monitoring bone density.
Consider osteoporosis-specific medications if bone mass remains low or fracture risk is high.
14.5 The Risk of Overlooking Secondary Causes
Leads to persistent bone loss despite therapy.
May delay diagnosis of serious underlying diseases (e.g., cancer, endocrine tumors).
Can result in avoidable fractures and poor long-term outcomes.
✅ Key Takeaway:
Secondary osteoporosis isn’t rare — it’s often hiding in plain sight.
A thorough evaluation, especially in men, premenopausal women, and younger patients, is vital. Treating the cause can sometimes restore bone strength and dramatically reduce fracture risk.
15: Fracture Risk Assessment — Tools and Strategies
When it comes to osteoporosis, bone density alone doesn’t tell the whole story.
Two patients with the same bone density can have very different fracture risks due to differences in age, medical conditions, bone quality, and even how often they fall.
That’s why comprehensive fracture risk assessment is essential for making better treatment decisions.
15.1 Why Fracture Risk Matters More Than Just BMD
BMD (Bone Mineral Density) is a strong predictor, but not the only predictor of fracture risk.
Factors such as:
Age (older = higher risk even with same BMD).
History of prior fracture.
Steroid use.
Family history of hip fracture.
Frequent falls.
A “normal” or “osteopenic” BMD doesn’t mean you’re safe — most fragility fractures actually happen in people with osteopenia, not full osteoporosis.
15.2 Key Assessment Tools
A. FRAX® (Fracture Risk Assessment Tool)
Developed by the WHO Collaborating Centre for Metabolic Bone Diseases.
Estimates 10-year probability of:
Hip fracture.
Major osteoporotic fracture (hip, clinical spine, humerus, forearm).
Inputs:
Age, sex, weight, height.
Previous fracture.
Parental hip fracture.
Smoking status.
Glucocorticoid use.
Rheumatoid arthritis.
Secondary osteoporosis causes.
Alcohol intake.
Optional: BMD T-score (femoral neck).
Advantages:
Widely validated across populations.
Helps guide treatment decisions in borderline BMD cases.
Limitations:
Doesn’t include fall history.
Not perfect for very young or very old patients.
B. QFracture®
Developed in the UK, includes more variables than FRAX:
Falls history.
Certain chronic illnesses.
Detailed medication use.
Predicts 1–10 year risk.
Advantage: Captures fall risk factors.
Limitation: Primarily validated in UK populations.
C. Garvan Fracture Risk Calculator
Developed in Australia.
Inputs:
Age, sex, weight.
BMD or body weight.
Falls in the past 12 months.
Fracture history.
Good for including fall risk as a major variable.
D. Other Screening Tools
Osteoporosis Self-assessment Tool (OST):
Simple formula based on age and weight to decide who needs DXA.
FRAMO Index: Focuses on fracture risk in older adults.
Trabecular Bone Score (TBS):
Derived from DXA scans — assesses bone quality rather than just quantity.
15.3 Key Risk Factors Beyond the Tools
Even if a calculator says your 10-year risk is “low,” you still need clinical judgment.
Frequent falls — especially in frail elderly.
Poor balance — vestibular or neurological conditions.
Low muscle mass (sarcopenia).
Vision problems.
Environmental hazards — poor lighting, loose rugs, lack of support rails.
15.4 How Clinicians Use Risk Scores
Low risk: Lifestyle modification, monitoring.
Moderate risk: Consider pharmacologic therapy if risk factors are present.
High risk: Initiate pharmacologic treatment promptly, plus fall prevention strategies.
Very high risk: Aggressive treatment, possibly anabolic agents.
15.5 Combining Tools with Clinical Judgment
Calculators are guides, not dictators.
Some patients need treatment even if scores are low:
Recent fragility fracture.
Ongoing high-dose steroid use.
Extremely low BMD at the spine or hip.
Others may not need treatment despite high scores if:
Short life expectancy.
Contraindications to medication.
Patient preference after informed discussion.
✅ Key Takeaway:
Fracture risk assessment is about looking beyond the numbers.
By combining BMD results, validated risk tools, and real-world clinical judgment, we can identify patients who truly need intervention — and tailor the approach to their actual risk.
16: The Silent Fractures — Vertebral Collapse and Its Hidden Toll
When people think of osteoporosis-related fractures, they often picture broken hips or wrists.
But the most common — and most overlooked — are vertebral compression fractures (VCFs).
These fractures happen in the spine, often with no major trauma, and can remain undetected for years while causing progressive damage.
16.1 What Is a Vertebral Compression Fracture?
A VCF occurs when one or more vertebral bodies collapse or lose height due to weakened bone.
Usually involves the thoracic spine (mid-back) or lumbar spine (lower back).
Collapse can be:
Mild: Only a slight reduction in vertebral height.
Severe: Wedge-shaped vertebra causing visible spinal curvature.
16.2 Why They’re Called “Silent”
Two-thirds of VCFs cause no obvious symptoms.
They may occur during:
Lifting a light object.
Bending forward.
Even coughing or sneezing.
Often missed on X-rays if imaging isn’t specifically reviewed for height loss.
Many are only discovered incidentally during scans for other reasons.
16.3 The Hidden Toll
Even without acute pain, VCFs can:
Cause gradual height loss (over months or years).
Lead to kyphosis (forward rounding of the spine), also known as a dowager’s hump.
Reduce lung capacity by compressing the chest cavity.
Increase risk of future fractures — one vertebral fracture doubles the risk of another.
Cause chronic pain due to muscle fatigue and nerve irritation.
16.4 Symptoms When They’re Not Silent
When a VCF is symptomatic, patients may experience:
Sudden mid-back pain that worsens with movement.
Pain that improves when lying down.
Muscle spasms near the fracture site.
Reduced spinal flexibility.
In severe cases, nerve compression symptoms (numbness, tingling, weakness).
16.5 Risk Factors Specific to VCFs
While general osteoporosis risk factors apply, VCFs are particularly common in:
Postmenopausal women (estrogen decline weakens bone structure).
Older adults with advanced age-related bone loss.
Chronic steroid users (medications like prednisone accelerate bone fragility).
People with prior vertebral fractures (strong predictor of recurrence).
Individuals with low body weight (less bone mass to lose).
16.6 Diagnosis
X-ray: Initial imaging, but can miss mild fractures.
MRI: Differentiates old vs. new fractures by detecting bone marrow swelling.
CT scan: Provides detailed bone architecture.
DXA-based Vertebral Fracture Assessment (VFA):
Low-radiation scan during a bone density test.
Can detect asymptomatic fractures.
16.7 Consequences of Missed Diagnosis
Untreated VCFs can lead to progressive spinal deformity.
Increases fall risk due to altered balance.
May cause psychological effects:
Low self-esteem.
Social withdrawal due to posture changes.
Cascade effect: One fracture leads to posture change → altered weight distribution → higher risk for additional fractures.
16.8 Treatment Approaches
Acute management:
Pain control (NSAIDs, acetaminophen, or short-term opioids).
Back bracing (temporary, not long-term).
Activity modification (avoid heavy lifting, twisting).
Long-term management:
Osteoporosis treatment (bisphosphonates, anabolic agents).
Postural training and physical therapy.
Fall prevention strategies.
Procedural options (selected cases):
Vertebroplasty: Injection of bone cement into fractured vertebra.
Kyphoplasty: Similar to vertebroplasty but with balloon inflation to restore height before cement injection.
Both are controversial — generally reserved for severe pain not responding to conservative treatment.
16.9 Prevention of Silent Fractures
Early osteoporosis screening (especially postmenopausal women over 50).
Routine spine imaging for those with:
Sudden height loss.
Unexplained back pain.
Prior fracture history.
Targeted therapy in high-risk groups before the first fracture occurs.
✅ Key Takeaway:
Vertebral compression fractures are the hidden epidemic of osteoporosis.
They may be painless, but their long-term consequences are life-changing — from posture changes and breathing problems to a significantly higher risk of future fractures.
Early detection through proactive screening can stop the silent damage before it becomes irreversible.
17: Hip Fractures — The Turning Point in Osteoporosis
Among all osteoporosis-related fractures, hip fractures are the most feared.
They represent a medical and social turning point for many patients — often marking the beginning of a rapid decline in mobility, independence, and overall health.
While the hip is a strong joint, in weakened bones it can fail from a simple fall or even a sudden twist.
17.1 Anatomy of the Hip Joint and Fracture Sites
The hip joint is a ball-and-socket articulation between:
Femoral head (the ball).
Acetabulum of the pelvis (the socket).
Osteoporosis-related fractures usually occur in the proximal femur:
Femoral neck fractures — between the ball and the shaft; prone to poor healing due to reduced blood supply.
Intertrochanteric fractures — between the femoral neck and shaft; generally better healing potential.
Subtrochanteric fractures — just below the trochanters; less common but more severe.
17.2 Why Hip Fractures Are a Game-Changer
High mortality rate:
20–30% of patients die within 1 year of a hip fracture, often due to complications like pneumonia, infections, or heart failure.
Loss of independence:
Only 40% regain their pre-fracture mobility.
Many require long-term care facilities.
Functional decline:
Reduced ability to walk, bathe, cook, or shop.
Psychological impact:
Depression and anxiety are common due to fear of falling again.
17.3 Mechanisms of Injury
In osteoporosis, minor trauma can cause a hip fracture:
Low-energy falls (especially sideways onto the hip).
Sudden pivoting or twisting movements.
In rare cases, spontaneous fractures occur without a fall.
17.4 Risk Factors Beyond Bone Density
While low bone mineral density (BMD) is central, other factors make hip fractures more likely:
Balance and gait problems (neurological disorders, muscle weakness).
Poor vision (cataracts, macular degeneration).
Environmental hazards (loose rugs, poor lighting).
Medications causing dizziness (sleep aids, sedatives).
History of prior falls.
17.5 Immediate Signs and Symptoms
Inability to bear weight.
Severe hip or groin pain.
Leg appears shortened and rotated outward.
Bruising or swelling around the hip.
In some impacted fractures, pain may be mild but worsens with movement.
17.6 Diagnosis
X-ray: First-line and usually definitive.
MRI: Detects occult fractures when X-ray is negative but suspicion is high.
CT scan: Used for complex fracture patterns.
17.7 Management — A Surgical Emergency
Hip fractures almost always require urgent surgical intervention within 24–48 hours:
Internal fixation: Screws, rods, or plates to stabilize the bone.
Hemiarthroplasty: Replacing the fractured femoral head.
Total hip arthroplasty: Replacing both ball and socket — often for patients with pre-existing arthritis.
Delay in surgery increases complications such as:
Deep vein thrombosis (DVT).
Pulmonary embolism.
Pneumonia.
Muscle wasting.
17.8 Postoperative Recovery
Early mobilization (within 24 hours) reduces mortality and improves recovery.
Physical therapy focuses on:
Gait training with a walker or crutches.
Muscle strengthening.
Fall prevention strategies.
Nutritional optimization (protein, calcium, vitamin D).
17.9 Prevention — Breaking the Chain Before It Starts
Fall prevention programs: Home safety assessments, balance training, vision correction.
Hip protectors: Padded garments to absorb impact.
Bone-strengthening therapy: Bisphosphonates, denosumab, teriparatide.
Addressing sarcopenia: Resistance training to maintain muscle strength.
17.10 Long-Term Outlook
Even after successful surgery, hip fractures often shorten life expectancy.
Patients with one hip fracture are at double the risk for a fracture in the other hip.
Lifelong osteoporosis management is essential to prevent recurrence.
✅ Key Takeaway:
A hip fracture is more than a broken bone — it’s a turning point in health.
It signals advanced bone fragility and often results in permanent lifestyle changes.
Early osteoporosis treatment, fall prevention, and prompt surgical care are the three pillars in preventing hip fractures from becoming life-ending events.
18: Wrist and Forearm Fractures — The Early Warning Signs
While hip fractures often mark the final stage of osteoporosis-related injury, wrist and forearm fractures are frequently the first alarm bell.
They can occur many years before hip or vertebral fractures, providing a valuable opportunity for early diagnosis and intervention.
Ignoring these early signs can allow bone loss to progress silently until a major, life-changing fracture occurs.
18.1 Why the Wrist is Vulnerable
The wrist is a complex joint formed by the distal radius, ulna, and eight small carpal bones.
In osteoporosis:
The distal radius (near the thumb side) becomes thinner and weaker.
Falls onto an outstretched hand — a common instinctive reaction — transfer the full force to the fragile bone.
Loss of trabecular bone in the metaphyseal region reduces shock absorption.
18.2 The Colles’ Fracture — A Classic Presentation
The Colles’ fracture is the most common osteoporotic wrist fracture:
Break occurs about 2.5 cm from the end of the radius.
The fractured fragment tilts upward, giving the “dinner fork” deformity.
Often occurs after a simple fall while walking.
18.3 Early Warning Role
Research shows:
Women who sustain a wrist fracture after menopause have double the risk of future hip or vertebral fractures.
Wrist fractures typically occur 10–15 years before hip fractures in the same patient.
This makes them an ideal trigger for BMD testing and osteoporosis treatment.
18.4 Risk Factors
Age-related bone loss (especially postmenopausal women).
Low muscle mass and weak grip strength.
Poor balance or reflexes, leading to falls.
Vitamin D deficiency reducing bone mineralization.
Previous history of minor fractures.
18.5 Symptoms
Sudden, sharp wrist pain after a fall.
Swelling and tenderness.
Visible deformity in severe cases.
Reduced range of motion.
Difficulty gripping or lifting objects.
18.6 Diagnosis
X-ray: Identifies fracture location, angulation, and displacement.
Bone density scan (DXA): Recommended after any low-trauma wrist fracture in adults over 50.
Laboratory tests: Calcium, vitamin D, thyroid, and parathyroid levels to detect underlying causes.
18.7 Treatment
Non-Surgical (Stable Fractures)
Immobilization in a cast or splint for 4–6 weeks.
Pain control and elevation to reduce swelling.
Early finger and elbow movement to avoid stiffness.
Surgical (Unstable or Displaced Fractures)
Open reduction and internal fixation (ORIF): Plates, screws, or pins to realign bones.
External fixation in severe cases with poor soft-tissue condition.
18.8 Recovery and Rehabilitation
Physical therapy to restore wrist flexibility, grip strength, and fine motor skills.
Gradual weight-bearing exercises after healing.
Addressing fear of falling through balance training.
18.9 Prevention
Fall-proofing the home: Remove loose rugs, improve lighting, use non-slip footwear.
Grip-strength training: Improves hand reflexes and reduces fall impact.
Osteoporosis treatment: Starting medications after a wrist fracture can prevent future major fractures.
Vitamin D and calcium supplementation for bone support.
18.10 Key Clinical Insight
A low-trauma wrist fracture in an older adult is never just an accident — it’s an important clinical red flag.
Treating the fracture without addressing the underlying bone weakness misses the opportunity to prevent devastating hip or spine fractures in the future.
✅ Key Takeaway:
Wrist and forearm fractures are the canary in the coal mine for osteoporosis.
If recognized early and followed by comprehensive osteoporosis management, they can prevent a patient from ever experiencing a life-changing fracture.
19: Vertebral Fractures — The Silent Crippler
Among all osteoporotic fractures, vertebral fractures are the most underdiagnosed yet the most physically and functionally devastating over time.
Often occurring without a major fall, they can go unnoticed for years — silently altering posture, compressing internal organs, and leading to chronic pain and disability.
19.1 Why Vertebrae Are So Vulnerable in Osteoporosis
The vertebral column is made up of 33 bones (24 movable vertebrae plus fused sacrum and coccyx).
The thoracic and lumbar vertebrae bear much of the body’s weight.
In osteoporosis:
The trabecular bone inside vertebrae becomes thinner and weaker.
The outer cortical shell cannot withstand normal daily loads.
Even minimal stresses — bending forward, lifting groceries, coughing, or sneezing — can cause compression fractures.
19.2 The “Silent” Nature
Up to two-thirds of vertebral fractures are never clinically diagnosed because:
Pain may be mild or dismissed as “back strain.”
Symptoms can appear weeks or months later.
Some are only discovered incidentally during X-rays for unrelated problems.
19.3 Typical Locations
Thoracic spine (T7–T8)
Thoracolumbar junction (T12–L1)
Lumbar spine (L2–L4)
These regions endure the highest mechanical stress.
19.4 Types of Vertebral Fractures
Wedge fracture – The front of the vertebra collapses, creating a forward tilt.
Biconcave fracture – The middle of the vertebra is depressed.
Crush fracture – Entire vertebra loses height.
19.5 Early Signs and Symptoms
Sudden, sharp back pain (especially after bending or lifting).
Height loss (≥ 3 cm compared to young adult height).
Progressive kyphosis (rounded upper back, “dowager’s hump”).
Limited spinal flexibility.
Fatigue from carrying weight in a shifted posture.
In severe cases — breathing restriction and abdominal crowding.
19.6 Complications Beyond the Spine
Reduced lung capacity due to compressed chest cavity.
Gastrointestinal issues like early satiety, constipation, or reflux from abdominal compression.
Reduced mobility and increased fall risk.
Increased mortality — especially if multiple vertebrae are involved.
19.7 Diagnosis
Imaging
X-ray: First-line for detecting vertebral height loss (≥20% height reduction defines fracture).
MRI: Differentiates recent vs. old fractures and detects spinal cord compression.
CT scan: For detailed bone morphology.
Vertebral Fracture Assessment (VFA): A low-radiation scan often performed alongside DXA.
19.8 Treatment
Acute Management
Pain control: NSAIDs, acetaminophen, or short-term opioids.
Bracing: Supports posture and reduces mechanical stress during healing.
Activity modification: Avoid heavy lifting, bending, or twisting.
Interventional
Vertebroplasty: Cement injection into fractured vertebra to stabilize it (now used selectively due to mixed outcomes).
Kyphoplasty: Balloon-assisted restoration of height before cement injection.
19.9 Rehabilitation
Postural training to reduce kyphosis progression.
Core and back muscle strengthening to improve spinal stability.
Balance exercises to prevent future falls.
Nutritional optimization — calcium, vitamin D, protein.
19.10 Prevention After the First Vertebral Fracture
The first vertebral fracture increases the risk of another fivefold within a year.
Therefore:
Start anti-osteoporotic medication immediately.
Reassess bone density and secondary causes.
Implement fall-prevention and spine-sparing strategies.
✅ Key Takeaway:
Vertebral fractures are not just a back problem — they are a systemic warning sign of severe bone fragility.
Detecting and treating them promptly can preserve posture, lung function, independence, and quality of life.
20: Glossary (Plain-English)
This glossary provides simple, plain-language explanations for all key terms used throughout the guide.
The definitions are brief but precise, making complex medical language accessible without losing accuracy.
A
Acetaminophen – A common pain reliever and fever reducer (also called paracetamol).
Acute – Sudden in onset and often short in duration.
Anti-osteoporotic medication – Drugs that slow bone loss or increase bone formation (e.g., bisphosphonates, denosumab).
B
Balance exercises – Physical activities that improve stability and prevent falls (e.g., Tai Chi).
Biconcave fracture – A vertebral fracture where the middle part of the vertebra collapses, giving it a “concave” appearance on both top and bottom surfaces.
Bisphosphonates – Medications that slow down bone breakdown by inhibiting bone-resorbing cells (osteoclasts).
Bone density – A measure of how strong and mineral-rich bones are.
Bone mineral density (BMD) – The amount of mineral matter per square centimeter of bone, measured by DXA scans.
Bracing – Wearing a supportive device to stabilize the spine or other body parts during healing.
C
Calcium – A mineral essential for bone strength and many body functions.
Cement injection (vertebroplasty/kyphoplasty) – A procedure where medical-grade cement is injected into a fractured vertebra to stabilize it.
Chronic – Lasting a long time, often for life.
Compression fracture – A break in a vertebra caused by pressure, often leading to loss of height in the bone.
Core muscles – The deep muscles of the abdomen, back, and pelvis that provide stability to the spine.
D
DXA (Dual-energy X-ray Absorptiometry) – A scan that measures bone mineral density to diagnose osteoporosis.
Dowager’s hump – A rounded upper back caused by multiple vertebral fractures.
E
Early satiety – Feeling full after eating only a small amount of food.
Epidemiology – The study of how often diseases occur in different groups of people and why.
F
Fall prevention – Strategies to reduce the risk of falling, including home safety modifications, exercise, and balance training.
Fracture risk – The likelihood of breaking a bone within a given period, often calculated using tools like FRAX.
G
Gastrointestinal issues – Problems related to the stomach and intestines, such as constipation or reflux.
Grip strength – The force your hand can apply when holding something; often used as a measure of overall muscle health.
H
Height loss – A reduction in standing height, often due to vertebral fractures.
Hormone therapy – Treatment using hormones to manage conditions like menopause or low testosterone.
K
Kyphoplasty – A minimally invasive surgery where a balloon is used to restore vertebral height before cement injection.
Kyphosis – Forward rounding of the upper back.
L
Lumbar spine – The lower part of the spine, consisting of 5 vertebrae (L1–L5).
M
MRI (Magnetic Resonance Imaging) – A scan that uses magnetic fields to create detailed images of body tissues.
Muscle strengthening – Exercises that improve the force and endurance of muscles.
N
NSAIDs (Nonsteroidal Anti-inflammatory Drugs) – Medications like ibuprofen or naproxen that reduce pain, fever, and inflammation.
O
Osteoblasts – Cells that build new bone tissue.
Osteoclasts – Cells that break down old bone tissue.
Osteoporosis – A disease where bones become weak and more likely to break.
P
Postural training – Exercises to improve body alignment and reduce abnormal spine curves.
Protein – A nutrient essential for muscle, bone, and overall health.
R
Rehabilitation – The process of regaining strength, mobility, and function after an injury.
Risk factors – Conditions or habits that increase the likelihood of disease or injury.
S
Sacrum – A triangular bone at the base of the spine.
Secondary osteoporosis – Bone loss caused by another medical condition or medication.
Spinal flexibility – The ability of the spine to bend and twist without pain or restriction.
T
Thoracic spine – The middle portion of the spine, consisting of 12 vertebrae (T1–T12).
Trabecular bone – The spongy inner layer of bone that gives strength while remaining lightweight.
V
Vertebrae – The small bones that form the spine.
Vertebral fracture assessment (VFA) – A scan to detect vertebral fractures, often done alongside bone density testing.
Vitamin D – A nutrient essential for calcium absorption and bone health.
✅ Key Takeaway:
The glossary turns complex medical terms into clear, understandable language, ensuring that both patients and general readers can follow the full guide without confusion.