Stomach Ulcers: Causes, Complications, and Modern Treatment Plans
"Discover everything you need to know about stomach ulcers in this comprehensive, easy-to-read guide. Written in a professional yet friendly style, this in-depth article explores the real causes of stomach ulcers, the latest scientific findings, potential complications, and cutting-edge treatment options. Whether you're a patient, caregiver, or curious reader, you'll gain valuable knowledge backed by trusted medical sources — all explained in clear, simple language that makes complex science easy to understand."
DISEASES
8/14/20259 min read
Stomach Ulcers: Causes, Complications, and Modern Treatment Plans
A friendly, yet deeply referenced, guide written as if by a specialist—so anyone can follow along.
Quick Overview (TL;DR)
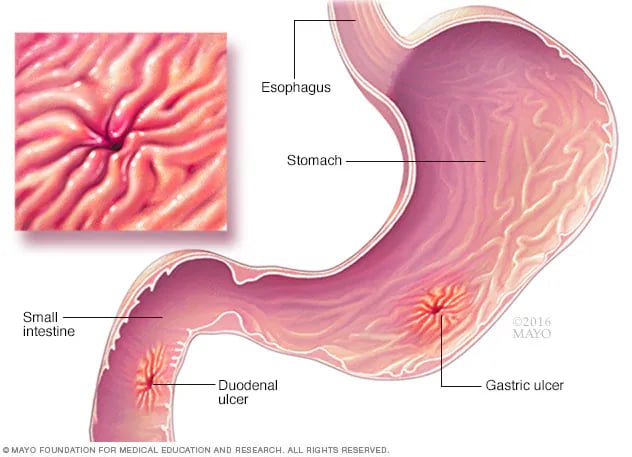
What they are: Stomach ulcers (gastric ulcers) are open sores in the stomach lining; ulcers can also live next door in the duodenum (duodenal ulcers). Together they’re called peptic ulcers. NIDDK
Main causes:
infection with Helicobacter pylori (H. pylori) and
long-term or high-dose NSAIDs (like ibuprofen, naproxen, or aspirin). Stress and spicy foods may worsen symptoms but don’t typically cause ulcers. NIDDKMayo Clinic
Why they matter: Ulcers can bleed, perforate (create a hole), or block the stomach outlet; bleeding may be life-threatening. docs.bvsalud.org
Good news: Today, most ulcers heal with acid suppression (PPIs/PCABs) and, if needed, antibiotics to eradicate H. pylori—guided by 2024 ACG and 2022 Maastricht consensus recommendations. socgastro.org.brAmerican College of GastroenterologyGut
Contents
Definitions & Anatomy (What exactly is a “stomach ulcer”?)
How Common Are Ulcers? (And what about H. pylori?)
Why Ulcers Happen: Causes and Risk Factors
Symptoms—From “silent” to dramatic
When to Seek Urgent Care
How Doctors Diagnose Ulcers and H. pylori
Complications (Bleeding, perforation, obstruction)
Modern Treatment Plans
Acid suppression (PPIs vs. PCABs / vonoprazan)
H. pylori eradication (best-practice regimens in 2024–2025)
NSAID-related ulcers (and what to do if you need pain meds)
Ulcer bleeding: hospital management
Diet, Lifestyle & Evidence-Based “Natural” Adjuncts
Prevention & Recurrence—Keeping ulcers gone
Special Situations (older adults, anticoagulants, pregnancy, bariatric surgery, Zollinger-Ellison)
Myths vs. Facts
Research Frontiers and What’s New
Doctor’s Visit Cheat Sheet (what to ask, what to bring)
References & Resources
1) Definitions & Anatomy
A peptic ulcer is an open sore in the lining of the stomach (gastric ulcer) or duodenum (duodenal ulcer). Ulcers form when the protective mucus barrier is overwhelmed by acid/pepsin and other injurious factors—most famously H. pylori and NSAIDs. NIDDKAmerican College of Gastroenterology
Gastric vs. duodenal in everyday terms:
Gastric ulcers sit in the stomach and sometimes hurt more with meals.
Duodenal ulcers are just beyond the stomach; classically the pain improves while eating and worsens a few hours later. (Patterns vary person to person.)
2) How Common Are Ulcers? (And what about H. pylori?)
H. pylori is one of the most common infections worldwide. Prevalence varies by region and age: roughly 20–35% in North America, higher in many developing regions (often 50–90%). Canada.ca
Global estimates show H. pylori prevalence has gradually declined in recent decades, but remains widespread. Gastro Journal
H. pylori is a major driver of peptic ulcers, gastric cancer, and gastric MALT lymphoma risk over the long term. Cancer.gov
3) Why Ulcers Happen: Causes and Risk Factors
The Big Two
H. pylori infection
This spiral-shaped bacterium colonizes the stomach, weakens mucosal defenses, and alters acid regulation. It’s the most important infectious cause of ulcer disease worldwide. Modern guidelines treat H. pylori eradication as essential whenever detected. Gutsocgastro.org.brNSAIDs (and aspirin)
These medications block prostaglandins that normally protect the stomach lining. Higher dose, longer duration, older age, corticosteroid or anticoagulant co-use, and prior ulcer all magnify risk. NIDDK
Other/less common contributors
Physiologic stress (e.g., critical illness) can cause “stress ulcers” in hospitalized patients.
Hypersecretory states (e.g., Zollinger-Ellison syndrome). Mayo Clinic
Rare infections or medications (e.g., combined corticosteroids with NSAIDs increasing risk). NIDDK
Smoking: slows healing and raises recurrence risk. Mayo Clinic
Myth check: Spicy foods and day-to-day stress don’t cause ulcers by themselves. They can aggravate symptoms while an ulcer is present. Mayo Clinic
4) Symptoms—From “Silent” to Dramatic
Many people have no symptoms (especially older adults or those on NSAIDs). When present, common symptoms include:
Gnawing/burning epigastric pain, often related to meals
Bloating, belching, heartburn
Nausea, sometimes vomiting
Night-time pain that wakes you up (common in duodenal ulcer) Cleveland Clinic
Alarm features that demand urgent evaluation:
Vomiting blood (red or coffee-grounds), black/tarry stools, fainting/dizziness, unintentional weight loss, trouble swallowing, or severe, sudden abdominal pain. Mayo Clinic
5) When to Seek Urgent Care
Seek emergency care immediately for:
Signs of bleeding: vomiting blood or passing black/tarry stools; weakness or fainting.
Sudden severe abdominal pain: worry for perforation.
Persistent vomiting or severe abdominal distension: possible gastric outlet obstruction.
These are classic ulcer complications that often require hospital care, endoscopy, and sometimes surgery. docs.bvsalud.org
6) How Doctors Diagnose Ulcers and H. pylori
A. Confirming an Ulcer
Upper endoscopy (EGD) is the gold standard: it visualizes the sore, allows biopsy (to rule out cancer for gastric ulcers), and enables endoscopic therapy if bleeding. NIDDK
B. Testing for H. pylori
Noninvasive tests: stool antigen or urea breath test (high accuracy).
Endoscopic tests: rapid urease test, histology, culture if needed.
Stop PPIs (usually for ~2 weeks) and bismuth/antibiotics (4 weeks) before testing to avoid false negatives—your clinician will guide timing. (This testing principle is reflected across guidelines and patient resources.) Gut
C. If H. pylori is Treated—Always Confirm Cure
Guidelines emphasize a test-of-cure (stool antigen or urea breath) ≥4 weeks after antibiotics and ≥2 weeks off PPIs whenever possible. socgastro.org.br
7) Complications: What Can Go Wrong?
Bleeding: The most frequent serious complication; may present with hematemesis, melena, weakness, or shock. Management follows rigorous protocols (resuscitation, risk scoring, PPIs, early endoscopy, targeted hemostasis). docs.bvsalud.org
Perforation: A hole through the stomach wall—sudden severe pain, peritonitis; surgical emergency. docs.bvsalud.org
Gastric outlet obstruction: Scarring or inflammation narrows the exit, causing vomiting and inability to tolerate food; may need endoscopic dilation or surgery after medical therapy. Mayo Clinic
8) Modern Treatment Plans
A. Turn Down the Acid: PPIs and PCABs
PPIs (omeprazole, esomeprazole, pantoprazole, etc.) are the cornerstone for ulcer healing—typically 4–8 weeks for uncomplicated ulcers; longer for complicated or NSAID-dependent cases. Mayo Clinic
PCABs (potassium-competitive acid blockers) like vonoprazan suppress acid faster and more potently than PPIs; they’re now FDA-approved in the U.S. (as Voquezna) and figure into modern H. pylori regimens. FDA Access DataU.S. Food and Drug Administration
Side-note on vonoprazan in the U.S.: FDA approvals cover Voquezna Dual Pak (vonoprazan + amoxicillin) and Voquezna Triple Pak (vonoprazan + amoxicillin + clarithromycin) for H. pylori (initial approval 2022; reformulated tablets 2023). U.S. Food and Drug AdministrationFDA Access DataDrugs.com
B. If H. pylori Is Present—Eradicate It (and choose wisely)
Why “choose wisely”? Because antibiotic resistance—especially to clarithromycin and levofloxacin—has surged, making older triple therapies unreliable in many settings. Modern recommendations from the American College of Gastroenterology (2024) and the Maastricht VI/Florence Consensus (2022) emphasize non-clarithromycin empiric regimens when susceptibility is unknown. socgastro.org.brAmerican College of GastroenterologyGut
First-line empiric options (adults, no penicillin allergy):
Optimized Bismuth-Based Quadruple Therapy (BQT) for 14 days
PPI + bismuth + tetracycline + metronidazole (or tinidazole). Remains the workhorse because it dodges clarithromycin resistance. socgastro.org.brAAFPVonoprazan–amoxicillin dual therapy for 14 days (PCAB dual) is a reasonable alternative in U.S. guidance; packaging may aid adherence, though cost and availability can be limiting. socgastro.org.brAmerican College of Gastroenterology
If penicillin-allergic:
Bismuth quadruple therapy (BQT) is usually preferred; consider formal penicillin allergy evaluation if history is uncertain, since amoxicillin-containing regimens are highly effective. American College of Gastroenterology
After failure of a first regimen (salvage therapy):
If BQT wasn’t used initially, use optimized BQT.
If BQT already failed, rifabutin-based triple therapy is suggested; consider culture-guided or molecular susceptibility testing if available. Pharmacy
Always confirm eradication with stool antigen or urea breath testing after therapy, timed appropriately (≥4 weeks post-antibiotics, ≥2 weeks off PPIs). socgastro.org.br
C. NSAID-Related Ulcers—When Pain Relief Is Non-Negotiable
Stop the NSAID if possible; if it must continue (e.g., for arthritis or cardiovascular aspirin), co-prescribe a daily PPI for prevention/healing.
Consider switching to a COX-2 selective agent plus PPI in high-risk patients, balancing cardiovascular risk.
H. pylori test-and-treat is recommended even in NSAID users, because co-existing infection increases ulcer risk and recurrence. (These strategies are consistent with major practice guidelines and reviews.) NIDDK
D. Ulcer Bleeding—What Happens in the Hospital?
The 2021 ACG Ulcer Bleeding Guideline (still current) lays out the roadmap:
Early risk stratification (e.g., Glasgow-Blatchford) to identify very-low-risk patients who might avoid admission.
Resuscitation and transfusion with a hemoglobin threshold around 7 g/dL in most patients.
High-dose PPI and early endoscopy (typically within 24 hours) for diagnosis and therapy (clips, thermal coagulation, injection, combinations).
Post-endoscopy PPI regimen to lower rebleeding risk. PubMeddocs.bvsalud.org
9) Diet, Lifestyle & Evidence-Based “Natural” Adjuncts
Diet: There’s no single “ulcer diet,” but patients often feel better by:
Eating smaller, more frequent meals; avoiding individual triggers (caffeine, alcohol, very spicy or high-fat meals).
Ensuring adequate protein, zinc, and vitamin C, which support healing (adjunctive evidence; not a substitute for medical therapy).
Do not smoke—it slows healing and ups recurrence. Mayo Clinic
Bismuth (as part of quadruple therapy or short-term symptomatic use) can help; zinc has limited supportive evidence as a healing adjunct in some contexts, but it’s not a primary treatment. Discuss supplements with your clinician, since they can interfere with testing (e.g., bismuth can affect H. pylori test accuracy shortly after use). Mayo Clinic
Probiotics: Some studies suggest they may reduce antibiotic side effects and possibly improve eradication rates modestly. They’re optional adjuncts—ask your doctor about strain and timing.
Coffee & spicy food: Not causes, but can exacerbate symptoms; personalize based on your triggers. Mayo Clinic
10) Prevention & Recurrence—Keeping Ulcers Gone
Treat H. pylori completely and verify cure. Recurrence drops dramatically once eradicated. socgastro.org.br
If you need NSAIDs/aspirin, review gastroprotection (PPI co-therapy) and dose with your clinician.
Avoid smoking, limit alcohol, and manage reflux/dyspepsia triggers.
Keep follow-up: gastric ulcers often get repeat endoscopy to document healing and exclude cancer (especially if any concerning features were present initially). Mayo Clinic
11) Special Situations
Older adults: More likely to have silent bleeding or present late; err on the side of early evaluation if new anemia, fatigue, or black stools. docs.bvsalud.org
Anticoagulants/antiplatelets: Ulcer bleeding risk increases; balancing thrombosis vs. bleeding requires individualized plans (PPI co-therapy is common). docs.bvsalud.org
Pregnancy: H. pylori testing/treatment is usually deferred unless clearly needed; always coordinate with obstetric care.
Post-bariatric surgery anatomy: Testing and access for endoscopy can be trickier—specialist involvement is key.
Zollinger-Ellison syndrome: Rare but important—think of it with multiple/refractory ulcers or severe esophagitis; managed with very potent acid suppression and tumor work-up. Mayo Clinic
12) Myths vs. Facts
“Stress and spicy foods cause ulcers.”
Myth. They can worsen symptoms but aren’t root causes. H. pylori and NSAIDs are the primary causes. NIDDKMayo Clinic“If my pain improves, the ulcer is gone.”
Not necessarily. Symptoms can come and go; always confirm H. pylori eradication and follow your clinician’s plan. socgastro.org.br“Old triple therapy works fine everywhere.”
Not anymore. Rising clarithromycin resistance has pushed guidelines toward bismuth quadruple therapy or vonoprazan-based regimens when susceptibility is unknown. socgastro.org.brAmerican College of Gastroenterology
13) Research Frontiers & What’s New
2024 ACG guidance stresses non-clarithromycin empiric therapy (e.g., 14-day BQT) and highlights PCAB-based regimens as practical options, with test-of-cure for everyone. socgastro.org.brAmerican College of Gastroenterology
Maastricht VI/Florence 2022 offers global perspective: treatment tailored to local resistance, broad indications to test-and-treat, and strong emphasis on eradication to prevent cancer. Gut
Vonoprazan (PCAB) momentum: Faster, stronger acid control; FDA-approved packs for H. pylori (dual and triple), with evolving roles in guidelines and real-world uptake. U.S. Food and Drug AdministrationFDA Access DataPMC
Evolving epidemiology: Global H. pylori prevalence is declining overall but remains high in many regions; public-health strategies for early detection/treatment are under discussion. Gastro Journal
14) Doctor’s Visit Cheat Sheet
Bring: medication list (especially NSAIDs, aspirin, anticoagulants), prior endoscopy reports, lab results.
Ask:
Do I need an endoscopy now?
How will we test for H. pylori, and when will we confirm eradication?
Which regimen fits my situation (BQT vs. PCAB dual/triple), and what side effects should I expect?
If I must take NSAIDs/aspirin, how do we protect my stomach?
What’s our plan to prevent recurrence and manage alarm symptoms?
15) References & High-Quality Resources
NIDDK (NIH) – Peptic Ulcers: definition, symptoms/causes, diagnosis. NIDDK+2NIDDK+2
Mayo Clinic – Peptic Ulcer: symptoms, diagnosis, treatment overview for patients. Mayo Clinic+1
ACG 2021 Ulcer Bleeding Guideline (Am J Gastroenterol): risk assessment, transfusion threshold, endoscopic therapy, PPI use. PubMeddocs.bvsalud.org
ACG 2024 H. pylori Treatment Guideline: empiric regimens (BQT first-line), test-of-cure, alternatives incl. rifabutin triple and PCAB dual. socgastro.org.brAmerican College of Gastroenterology
Maastricht VI/Florence 2022 Consensus (Gut): global recommendations on indications, diagnosis, treatment, and cancer prevention. Gut+1
AAFP 2023 Review: accessible summary aligning with major guidelines; BQT as first-line. AAFP
FDA & Labeling (Voquezna/vonoprazan): approvals and pack details for H. pylori. U.S. Food and Drug AdministrationFDA Access Data
WHO/NCI resources: H. pylori and cancer risk (including MALT lymphoma). Cancer.gov
Public Health Canada: practical prevalence snapshot by region (useful context). Canada.ca
A Step-By-Step Modern Care Pathway (Putting It All Together)
Initial evaluation: Identify alarm features. If present → urgent endoscopy. If not, consider noninvasive H. pylori testing and trial PPI based on age/risk. NIDDK
If H. pylori positive: Treat with 14-day BQT (empiric) or PCAB dual where appropriate; avoid clarithromycin regimens unless susceptibility known. Confirm eradication after treatment. socgastro.org.br
If NSAID-related: Stop NSAID if possible; if not, continue PPI and reassess pain strategy. Screen/treat H. pylori. NIDDK
For bleeding ulcers: Follow ACG 2021 hospital algorithm—resuscitate, risk-score, early endoscopy, hemostasis, high-dose PPI. docs.bvsalud.org
Follow-up: Repeat endoscopy for gastric ulcers when indicated, confirm cure of H. pylori, and solidify prevention (PPI for high-risk NSAID/antiplatelet users, smoking cessation). Mayo Clinic
Friendly Final Thoughts
Stomach ulcers can be scary, but modern care is precise, guideline-driven, and highly effective. The two biggest wins you can give yourself are:
Treat H. pylori fully and confirm the cure, and
If you need NSAIDs or aspirin, partner with your clinician on a protection plan (usually a daily PPI).
If you’d like, I can now:
Convert this into a downloadable Word or PDF (just say which),
Add a one-page patient handout, or
Tailor a treatment algorithm for a specific patient scenario (e.g., penicillin allergy, prior BQT failure, on anticoagulants).